Sporotrichosis is a subacute or chronic subcutaneous mycosis caused by thermodimorphic fungi of the genus Sporothrix.1 Although the diagnosis of the classic form is relatively straightfoward, other variants pose a significant diagnostic challenge. Morphologically, it can simulate keratoacanthoma, erysipelas, sarcoidosis and pyoderma gangrenosum (PG). The term pyoderma gangrenosum-like sporotrichosis (PGLS) is used to describe extensive ulcerative forms.2–11 Three new cases are reported and previously published cases are reviewed.
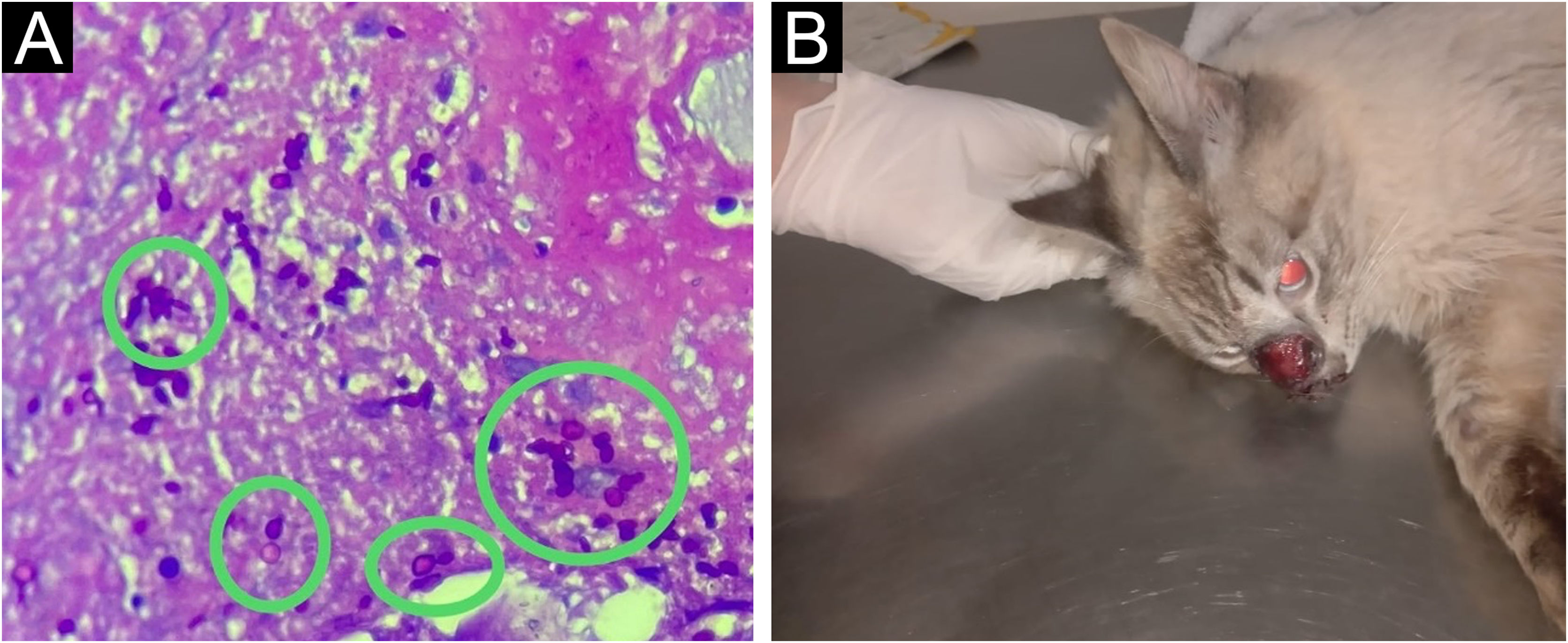
A 48-year-old female patient presented with a painful ulcer on her right thigh for three months, with progressive enlargement and satellite lesions (Fig. 1). She had autoimmune hepatitis and had been treated with prednisone 1 mg/kg/day and azathioprine 3 mg/kg/day for five years. Tissue cultures were negative, and histopathology had shown granulomatous, suppurative panniculitis and vascular aggression. Given the hypothesis of PG, the patient received intravenous pulse therapy with methylprednisolone (1 g/day for three days) without improvement. As there was no response, a new biopsy was performed on the edge of the same lesion, one week after pulse therapy. Yeast-like structures stained with PAS (periodic-acid Schiff) were found in the subcutaneous tissue on histopathology (Fig. 2A). Simultaneously, patient’s pet cat was diagnosed with sporotrichosis through secretion culture (Fig. 2B). As the patient had hepatorenal syndrome, treatment with potassium iodide (2 g/day) was chosen despite being immunosuppressed. The patient showed almost complete healing within three months of treatment (Fig. 1), when she presented decompensation of the liver condition and died. Although potassium iodide-associated hepatotoxicity is rare, it may occur in patients with pre-existing liver disease. However, the Gastroenterology team correlated the outcome to the worsening of the underlying disease.
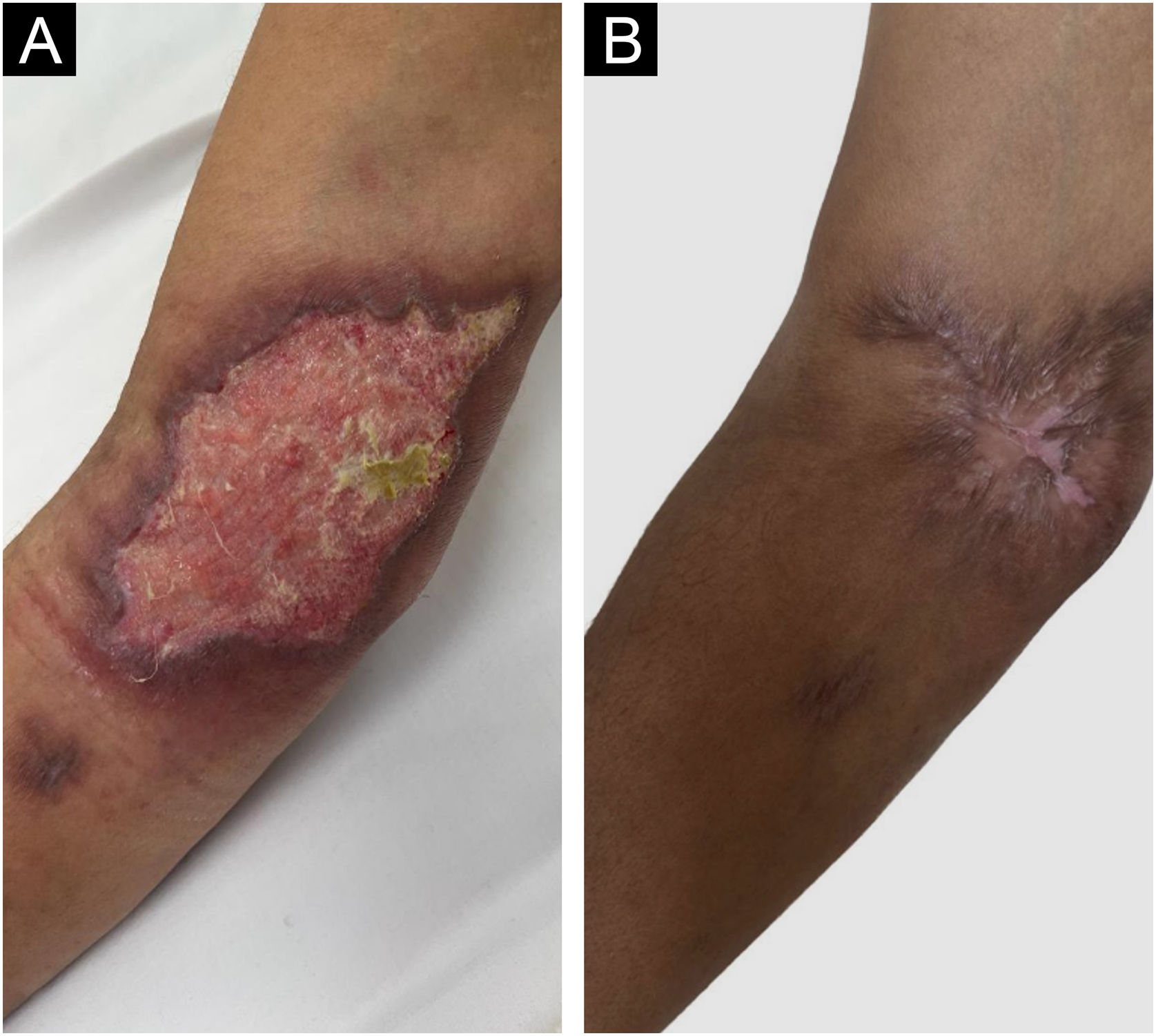
The second patient, a 49-year-old male, had a painful ulcer in the right antecubital fossa with satellite lesions and perilesional lymph node enlargement of one-month evolution (Fig. 3A). He had psoriatic arthritis and diabetes mellitus. He had been treated with infliximab 3 mg/kg for four years, sulfasalazine 2 g/day for three years, and prednisone 20 mg/day for six months. Based on the initial suspicion of ecthyma gangrenosum, clindamycin and ciprofloxacin were administered for one month, without improvement. Subsequently, Sporothrix sp. was isolated from the ulcer fragment and sent for culture. Histopathology revealed abscessed granulomas, but the fungal culture was negative. Itraconazole was started, but the patient developed hepatorenal syndrome, which led to drug discontinuation. As an alternative, potassium iodide (3 g/day) was administered for two months, with healing of the ulcer (Fig. 3B).
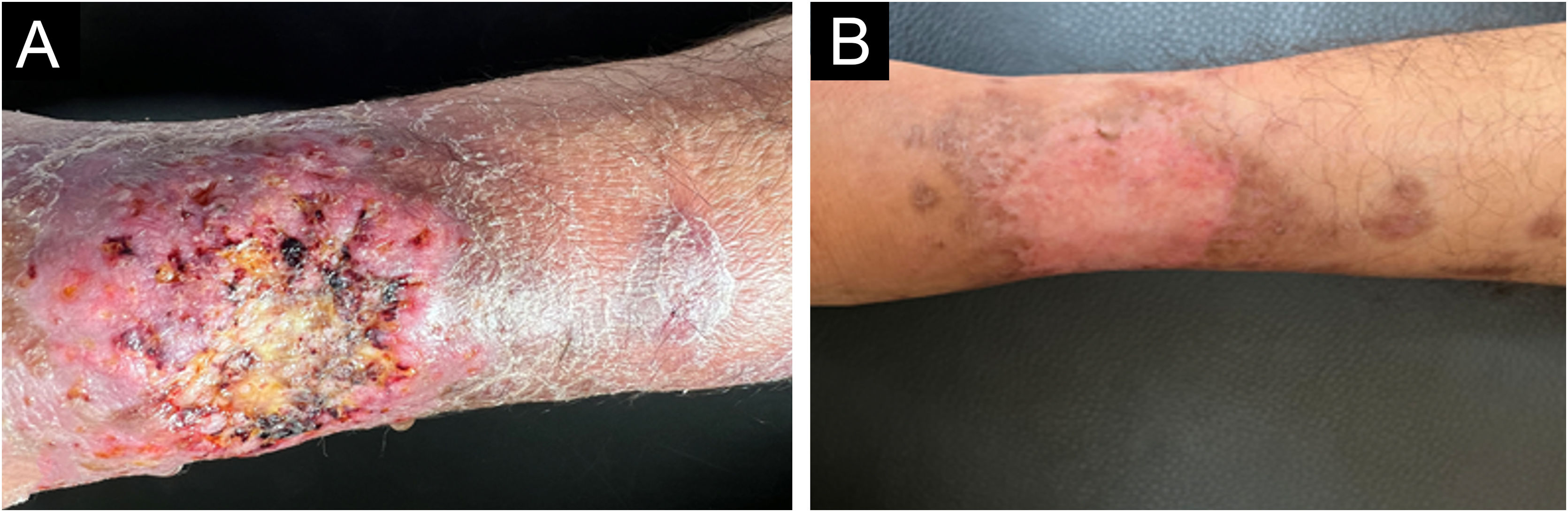
The third patient, a 39-year-old male individual, presented a painful, ulcerated lesion with a cribriform appearance and satellite abscessed papules and nodules on the left leg of three-week evolution (Fig. 4A). Initial treatment with amoxicillin combined with clavulanate, clindamycin, vancomycin, and cefepime yielded no improvement. The patient had Crohn's disease and had received methotrexate 20 mg/week for four years and infliximab 5 mg/kg for two years. Given the initial hypothesis of PG, dapsone 100 mg/day was added for 30 days. Histopathology showed a neutrophilic inflammatory infiltrate and leukocytoclasia, abscessed granulomas and rare yeast-like spindle-shaped structures. In the culture, there was Sporothrix sp. growth, confirming the diagnosis. Itraconazole (200 mg/day) and potassium iodide (2 g/day) were started concomitantly, with healing after four months (Fig. 4B).
Extensive ulcerative forms of sporotrichosis are rarely described and occur especially in immunosuppressed patients. The term PGLS has been adopted due to the clinical and histopathological similarities with PG: phagedenic ulcers with erythematous edges, cribriform morphology and neutrophilic infiltrate.3 The initial approach to PG requires the exclusion of differential diagnoses through biopsy and culture. However, the search for pathogens is not always positive at first. The lack of response to immunosuppressants should motivate a diagnostic review. Furthermore, fungal structures are difficult to observe, making the diagnosis of sporotrichosis even more difficult.3 In this context, the culture of secretions or tissue fragments is extremely important,11 as well as a detailed anamnesis, especially regarding the presence of felines and risk activities, such as gardening.
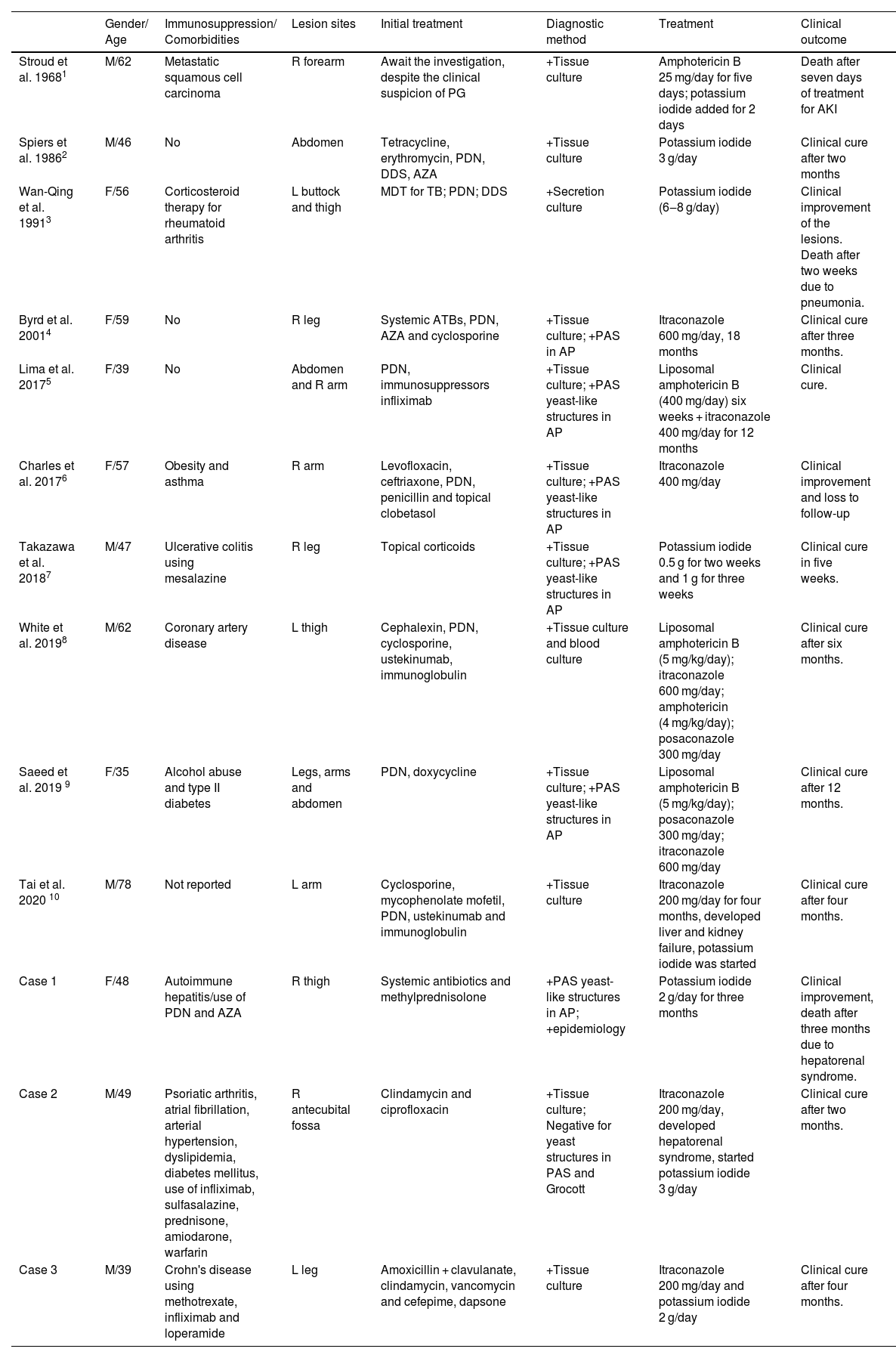
Only 10 published cases of PGLS were found in the English-language literature in PUBMED (Table 1). More than half (n = 6) were published in the last six years, which may reflect an improvement in diagnostic accuracy or an increase in incidence, mainly due to the growing population of immunosuppressed patients. The cases reported herein were under immunosuppression.
Cases published in the literature (PUBMED database, English language until July 2024).
| Gender/ Age | Immunosuppression/ Comorbidities | Lesion sites | Initial treatment | Diagnostic method | Treatment | Clinical outcome | |
|---|---|---|---|---|---|---|---|
| Stroud et al. 19681 | M/62 | Metastatic squamous cell carcinoma | R forearm | Await the investigation, despite the clinical suspicion of PG | +Tissue culture | Amphotericin B 25 mg/day for five days; potassium iodide added for 2 days | Death after seven days of treatment for AKI |
| Spiers et al. 19862 | M/46 | No | Abdomen | Tetracycline, erythromycin, PDN, DDS, AZA | +Tissue culture | Potassium iodide 3 g/day | Clinical cure after two months |
| Wan-Qing et al. 19913 | F/56 | Corticosteroid therapy for rheumatoid arthritis | L buttock and thigh | MDT for TB; PDN; DDS | +Secretion culture | Potassium iodide (6‒8 g/day) | Clinical improvement of the lesions. Death after two weeks due to pneumonia. |
| Byrd et al. 20014 | F/59 | No | R leg | Systemic ATBs, PDN, AZA and cyclosporine | +Tissue culture; +PAS in AP | Itraconazole 600 mg/day, 18 months | Clinical cure after three months. |
| Lima et al. 20175 | F/39 | No | Abdomen and R arm | PDN, immunosuppressors infliximab | +Tissue culture; +PAS yeast-like structures in AP | Liposomal amphotericin B (400 mg/day) six weeks + itraconazole 400 mg/day for 12 months | Clinical cure. |
| Charles et al. 20176 | F/57 | Obesity and asthma | R arm | Levofloxacin, ceftriaxone, PDN, penicillin and topical clobetasol | +Tissue culture; +PAS yeast-like structures in AP | Itraconazole 400 mg/day | Clinical improvement and loss to follow-up |
| Takazawa et al. 20187 | M/47 | Ulcerative colitis using mesalazine | R leg | Topical corticoids | +Tissue culture; +PAS yeast-like structures in AP | Potassium iodide 0.5 g for two weeks and 1 g for three weeks | Clinical cure in five weeks. |
| White et al. 20198 | M/62 | Coronary artery disease | L thigh | Cephalexin, PDN, cyclosporine, ustekinumab, immunoglobulin | +Tissue culture and blood culture | Liposomal amphotericin B (5 mg/kg/day); itraconazole 600 mg/day; amphotericin (4 mg/kg/day); posaconazole 300 mg/day | Clinical cure after six months. |
| Saeed et al. 2019 9 | F/35 | Alcohol abuse and type II diabetes | Legs, arms and abdomen | PDN, doxycycline | +Tissue culture; +PAS yeast-like structures in AP | Liposomal amphotericin B (5 mg/kg/day); posaconazole 300 mg/day; itraconazole 600 mg/day | Clinical cure after 12 months. |
| Tai et al. 2020 10 | M/78 | Not reported | L arm | Cyclosporine, mycophenolate mofetil, PDN, ustekinumab and immunoglobulin | +Tissue culture | Itraconazole 200 mg/day for four months, developed liver and kidney failure, potassium iodide was started | Clinical cure after four months. |
| Case 1 | F/48 | Autoimmune hepatitis/use of PDN and AZA | R thigh | Systemic antibiotics and methylprednisolone | +PAS yeast-like structures in AP; +epidemiology | Potassium iodide 2 g/day for three months | Clinical improvement, death after three months due to hepatorenal syndrome. |
| Case 2 | M/49 | Psoriatic arthritis, atrial fibrillation, arterial hypertension, dyslipidemia, diabetes mellitus, use of infliximab, sulfasalazine, prednisone, amiodarone, warfarin | R antecubital fossa | Clindamycin and ciprofloxacin | +Tissue culture; Negative for yeast structures in PAS and Grocott | Itraconazole 200 mg/day, developed hepatorenal syndrome, started potassium iodide 3 g/day | Clinical cure after two months. |
| Case 3 | M/39 | Crohn's disease using methotrexate, infliximab and loperamide | L leg | Amoxicillin + clavulanate, clindamycin, vancomycin and cefepime, dapsone | +Tissue culture | Itraconazole 200 mg/day and potassium iodide 2 g/day | Clinical cure after four months. |
PDN, Prednisone; AZA, Azathioprine; DDS, Dapsone; ATB, Antibiotics; PAS, Periodic Acid of Schiff; AP, Anatomopathological; MDT, Multi-drug therapy; TB, Tuberculosis; AKI, acute kidney insuficiency.
Interestingly, they had ulcers with a larger axis in the lymphatic drainage direction, while PG ulcers often have a more rounded shape. Satellite lesions occurred in the three cases and may help formulate the hypothesis of sporotrichosis.
Although potassium iodide is not the first therapeutic choice for immunosuppressed patients, it can be used as monotherapy when there are contraindications to other treatments.3,4 In view of the experience in the first two cases, due to the synergistic drug effect and the report of the emergence of itraconazole-resistant S. brasiliensis isolates,1 the association was chosen for the third patient.
Financial supportNone declared.
Authors' contributionsLucas Campos Garcia: Study design, critical review, drafting and editing of the manuscript, review of the literature, approval of the final version of the manuscript.
Marianne de Sousa Nunes Soares: Drafting and editing of the manuscript, review of the literature.
Gustavo Gomes Resende: Drafting and editing of the manuscript, review of the literature.
Luciana Baptista Pereira: Study design, critical review, drafting and editing of the manuscript, review of the literature, approval of the final version of the manuscript.
Conflicts of interestNone declared.
Study conducted at the Faculty of Medicine, Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil.