Background Stevens-Johnson syndrome and toxic epidermal necrolysis are life-threatening blistering drug reactions with high incidence of ocular sequela. The term ‘Epidermal Necrolysis’ has been recently used to better describe the full spectrum of the disease that includes Stevens-Johnson syndrome and toxic epidermal necrolysis at opposite ends, which differ by the extent of body surface area with epidermal detachment. SCORTEN is a mortality prognosis score for ‘Epidermal Necrolysis’ cases that still needed validation in acquired immunodeficiency syndrome.
Objective To evaluate the SCORTEN performance in acquired immunodeficiency syndrome, and the differences in outcomes between acquired immunodeficiency syndrome and non- acquired immunodeficiency syndrome cohorts.
Methods Retrospective cohort study of AIDS and non-AIDS ‘Epidermal Necrolysis’ cases admitted to a Brazilian reference center from 1990-2014.
Results Five deaths (16.7%) occurred as a consequence of EN in 30 AIDS patients, and seven (17.9%) in 39 non-AIDS patients, relative risk (RR) .92 (p=1.0). SCORTEN showed great performance, with an Area Under the Receiver Operating Curve (AUC) (ROC) of 0.90 with a 95% confidence interval ranging from .81 to .99. The performance of SCORTEN was better among non-AIDS patients than AIDS patients: AUC non- acquired immunodeficiency syndrome =0.99 (CI 05% 0.96-1.00), AUC acquired immunodeficiency syndrome = 0.74 (CI 95% 0.53-0.95), p=.02.
Study Limitations: Heterogeneity of cases, wide variation of systemic corticosteroid doses when used.
Conclusion: SCORTEN is valid for the Brazilian population, including among those patients with acquired immunodeficiency syndrome, and, as such, its use is recommended for aiding treatment choice in this subgroup of patients.
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are life-threatening blistering mucocutaneous reactions usually triggered by drug exposure.1 These diseases are now considered to be different points on the spectrum of a single disease, with TEN representing the most severe expression of the condition.2 The term ‘Epidermal Necrolysis’ (EN) has been recently used to better describe the full spectrum of disease that includes SJS and TEN at opposite ends, which differ only by the percentage of body surface area of epidermal detachment (SJS<10% and TEN>30%), and, therefore, by severity.3 Data suggest that the pathogenesis of EN is mediated by medication-induced cytotoxic response by T-cells triggered by drugs, which results in keratinocyte apoptosis,possibly due to modifications in major histocompatibility complex I proteins by non-covalent binding of the offending drug to specific human leucocyte antigens (HLA), leading to CD8+ T-cell activation.3-5
Despite being rare, this disease presents high lethality (12-46%),and high morbidity, with generalized infections, sepsis, and disseminated intravascular coagulation as the major acute adverse events, and ocular scars as main chronic sequela.3,6,7 The severity of such events imposes the significance of adequate management. Corticotherapy,8,9 intravenous immunoglobulin therapy,10,11 and cyclosporine-A12 have been proposed as treatments; however, there is still no consensus or guidelines about their use, nor satisfactory treatment trials to further evaluate the true impact of such therapies.4,8,13,14
Bastuji-Garin et al analyzed French patients diagnosed with EN and proposed a score to determine prognosis: the SCORTEN.15 (Table 1). This score was initially tested in France; however, it is known that the clinical management of EN patients may vary according to the country and hospital they are admitted to.8 It has been argued that this might render the SCORTEN less reliable when applied to different populations, thus invalidating studies that use it as a tool to predict mortality rates. Despite that, SCORTEN has been validated for its use in the United States of America,16 Korea,17 Canada,18 and China.19
SCORTEN – Score for Toxic Epidermal Necrolysis
| Risk factors add 1 point if present: | |
|---|---|
| · Detachable Skin Surface Area > 10% | |
| · neoplasia | · urea > 28mg/dL |
| · HR ≥ 120 bpm | · serum glucose > 252mg/dL |
| · age > 40 years | · bicarbonate < 20mEq/L |
| SCORTEN | Lethality (%) |
| 0-1 | 3.2 |
| 2 | 12.1 |
| 3 | 35.8 |
| 4 | 58.3 |
| ≥5 | 90 |
The purpose of this study was to evaluate the performance of SCORTEN as mortality predictor in acquired immunodeficiency syndrome (AIDS) and to analyze differences in outcomes between AIDS and non-AIDS Brazilian cohorts.
MethodsA retrospective cohort was performed by review of hospital charts. Patients included in this study were all those with or without AIDS, admitted to a tertiary level, university hospital in Brazil that fulfilled the criteria for clinical diagnosis of SJS-TEN20 All patients with dubious or incorrect diagnosis were excluded, such as no description of mucosal involvement, non-blistering exanthema, erythema multiforme, psoriasis, pemphigus vulgaris, bullous pemphigoid, and paraneoplastic pemphigus. After detailed screening, 86 patients were excluded from this study. This study was approved by two institutional research ethics review boards (HCRP #7737/2011; Plataforma Brasil: Opinion 1.425.047 UEPG; Opinion 1.428.738 HCFMRP-USP).
The collected data included human immunodeficiency virus (HIV) 1 and 2 serology, CD4, total viral load, length of hospitalization, cause of death, body surface area involvement, list of suspect triggering drugs, age, gender, year of diagnosis, comorbidities, alcohol and tobacco use. Analysis of the results of all blood tests performed during admission, such as biochemical, gasometrical, serological, hematological tests. Also, results of skin biopsies performed during admission, in-hospital medical prescriptions, necropsy charts and cause of death statement in the death certificate. Systemic corticosteroids (SCS) and intravenous immunoglobulin (IVIG) given during admission were considered despite dose. SCORTEN was calculated up to the fifth day of hospitalization as the highest sum of up to seven risk factors on the same day when present: age higher than 40 years, malignancy, tachycardia above 120bpm, detachable body surface area higher than 10%, serum urea levels higher than 28mg/dL, serum glucose levels higher than 252 mg/dL, and serum bicarbonate levels below 20mEq/L.21
Relative risk (RR) was obtained for comparison of risks among AIDS and non-AIDS population. The association between categorical variables was tested by Fisher’s exact test, and for continuous variables by Wilcoxon rank-sum Test. P-values under .05 were considered significant. The risk of death or long hospital stay (>28days) was tested through Poisson’s regression, reported as incidence rate ratio (IRR). The Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) curve was used to verify the predictive capacity of SCORTEN. AUC greater than 0.70 was considered the minimum acceptable accuracy. Besides being tested on the general population, the SCORTEN was tested among AIDS and non-AIDS patients separately. Statistical analyses were performed using the software Stata ® 14.2 – Statistics/Data analysis, StataCorp LP, Texas, USA.
ResultsSixty-nine patients were included in this study, with age varying between 1 and 74 years. Table 2 shows the different frequencies of the main studied variables among AIDS and non-AIDS patients. The distribution of cases through the years of admission is shown in figure 1, as well as SCORTEN, HIV, treatment and outcome. All 30 HIV-positive patients were classified as AIDS “C” patients, due to opportunistic infections denoting the severity of the immunodeficiency syndrome, two had CD4 levels between 200 and 500 cells/µL with clinical evidence of AIDS (AIDS C2), and the other 28 had CD4 count bellow 200 cells/µL (AIDS C3).
Characteristics of EN patients with and without Acquired Immunodeficiency Syndrome (AIDS) admitted to a tertiary university hospital in Brazil, from 1990 to 2014
| Total median (IR) | Non-AIDS median (IR) | AIDS median (IR) | p | |
|---|---|---|---|---|
| Age (years) | 32 (30) | 32 (46.5) | 32.5 (12.75) | 0.472 |
| Days of Hospitalization | 16 (17) | 13 (15) | 20 (17.75) | 0.116 |
| n (%) | n (%) | n (%) | ||
| Total | 69 (100) | 39 (100) | 30 (100) | .800 |
| Deaths † | 12 (17.4) | 7 (18) | 5 (16.7) | 1 |
| Stay length > 28 days | 17 (24.6) | 8 (20.5) | 9 (30) | .419 |
| Ocular sequelae | 11/57 (19.3) | 10/32 (31.2) | 1/25 (4) | .016* |
| Support treatment only | 35 (50.7) | 22 (56.4) | 13 (43.3) | .336 |
| Systemic corticotherapy | 30 (43.5) | 13 (33.3) | 17 (56.7) | .086 |
| IV immunoglobulin | 6 (8.7) | 4 (10.3) | 2 (6.7) | .690 |
| SCORTEN 0 | 3 (4.3) | 3 (7.7) | 0 (0) | .252 |
| SCORTEN 1 | 18 (26.1) | 11 (28.2) | 7 (23.3) | .784 |
| SCORTEN 2 | 18 (26.1) | 9 (23.1) | 9 (30) | .586 |
| SCORTEN 3 | 14 (20.3) | 6 (15.4) | 8 (26.7) | .336 |
| SCORTEN 4 | 11 (15.9) | 5 (12.8) | 6 (20) | .514 |
| SCORTEN 5 | 3 (4.3) | 3 (7.7) | 0 (0) | .252 |
| SCORTEN 6 | 1 (1.4) | 1 (2.7) | 0 (0) | 1 |
| SCORTEN 7 | 1 (1.4) | 1 (2.7) | 0 (0) | 1 |
| Neoplasia § | 3 (4.3) | 2 (2.9) | 1 (3.3) | 1 |
| BSA >10% § | 55 (79.7) | 29 (74.6) | 26 (86.7) | .242 |
| HR>120 bpm § | 16 (23.2) | 13 (33.3) | 3 (10) | .042* |
| Urea>28mg/dL § | 36 (52.2) | 20 (51.3) | 16 (53.3) | 1 |
| Serum glucose>252mg/dL § | 4 (5.8) | 4 (10.3) | 0 (0) | .127 |
| Bicarbonate<20mEq/L § | 27 (39.1) | 10 (25.7) | 17 (56.7) | .013* |
| >40 years S | 25 (36.2) | 17 (43.9) | 8 (26.7) | .207 |
| 13-40 years | 32 (46.4) | 11 (28.2) | 21 (70) | .012* |
| <13 years | 12 (17.4) | 11 (28.2) | 1 (3.3) | .012* |
| Male | 47 (68.1) | 26 (66.7) | 21 (70) | .800 |
| Female | 22 (31.9) | 13 (33.3) | 9 (30) | .800 |
| Drugs (all) | 63 (91.3) | 35 (89.7) | 28 (93.3) | .690 |
| ACE-inhibitors | 6 (8.7) | 5 (12.8) | 1 (3.3) | .223 |
| Antibiotics (all) | 37 (53.6) | 20 (51.3) | 17 (56.7) | .808 |
| Sulfonamides | 19(27.5) | 9 (23.1) | 10 (33.3) | .419 |
| Cephalosporins | 5 (7.2) | 3 (7.1) | 2 (6.7) | 1 |
| Quinolones | 1 (1.4) | 1 (2.7) | 0 (0) | 1 |
| Penicillins | 10 (14.5) | 8 (20.5) | 2 (6.7) | .168 |
| Tetracyclines | 1 (1.4) | 0 (0) | 1 (3.3) | .435 |
| Macrolides | 1 (1.4) | 0 (0) | 1 (3.3) | .435 |
| Anticonvulsive drugs (all) | 16 (23.2) | 10 (25.7) | 6 (20) | .775 |
| Phenobarbital | 5 (7.2) | 4 (10.3) | 1 (3.3) | .379 |
| Carbamazepine | 6 (8.7) | 5 (12.8) | 1 (3.3) | .223 |
| Phenytoin | 9 (13) | 5 (12.8) | 4 (13.3) | 1 |
| Allopurinol | 3 (4.3) | 3 (7.1) | 0 (0) | .252 |
| NSAIDs (all) | 10 (14.5) | 10 (15.7) | 0 (0) | .004* |
| Diclofenac | 5 (7.2) | 5 (12.8) | 0 (0) | .064 |
| HAART (all) | 10 (14.5) | 0 (0) | 10 (33.3) | <.001* |
Epidermal Necrolysis. Distribution of cases from a high complexity hospital in Brazil from January of 1990 to December of 2014. Triangles: Patients with Acquired Immunodeficiency Syndrome (AIDS). Circles: Patients without AIDS. X: death as direct consequence of SJS-TEN. Slash: death by unrelated cause. White: support treatment only. Grey: systemic corticotherapy. Black: IV immunoglobulin
The most frequent suspected offending drugs were: sulfonamides, 19 cases (27.5%); penicillins, 10 cases (14.5%), phenytoin, nine cases (13%); carbamazepine and imidazoles, six cases each (8.7%); cephalosporins, diclofenac, metamizole, and phenobarbital, five cases each (7.2%); allopurinol, three cases (4.3%) and tenoxicam, two cases (2.9%). Some drugs were associated with higher mortality rates, (Table 3). Patients who presented EN triggered by the use of cephalosporins had a rate (IRR) 11.85 higher for death, p=.008, with four deaths among five patients (lethality of 80%), being present in one third of the deaths in this study. It was the offending drug of the patients with SCORTEN 6 and 7, the highest scores in this study. Angiotensin converting enzyme inhibitors had an IRR for death of 14.5, p=.016, with three deaths among six patients. (Table 3).
Risk factors for death and long hospital stay (>28 days), among cases of epidermal necrolysis admitted to a tertiary level university hospital in Brazil, from 1990 to 2014, with incidence rate ratios obtained through Poisson’s regression
| Risk factors | Total n (%) | Deaths n (%) | IRR (95%CI) | p | Long Hospital Stay n (%) | IRR (95%CI) | p |
|---|---|---|---|---|---|---|---|
| AIDS | 28 (40.6) | 5 (17.8) | 2.02 (0.48-8.55) | .341 | 9 (32.1) | 1.60 (0.78-3.26) | 0.196 |
| Male | 47 (69.6) | 7 (16.7) | 0.63 (0.16-2.48) | .508 | 14 (29.2) | 1.40 (0.62-3.13) | 0.420 |
| Age > 40 | 25 (36.2) | 7 (28) | 1.31 (0.32-5.37) | .700 | 8 (32) | 1.23 (0.58-2.59) | 0.589 |
| Neoplasia | 3 (4.3) | 2 (66.7) | 2.96 (0.17-50.44) | .453 | 2 (66.7) | 1.82 (0.34-9.79) | 0.482 |
| Drugs | |||||||
| Cephalosporins | 5 (7.2) | 4 (80) | 11.85 (1.89-74.4) | .008* | 2 (40) | 1.15 (0.31-4.29) | .829 |
| ACEI | 6 (8.7) | 3 (50) | 14.48 (1.64-128.25) | .016* | 3 (50) | 1.41 (0.41-4.84) | .581 |
| Phenobarbital | 5 (7.2) | 1 (20) | 2.03 (0.11-35.94) | .629 | 3 (60) | 1.91 (0.57-6.42) | .296 |
| Phenytoin | 9 (13) | 2 (22.2) | 3.50 (0.42-29.29) | .248 | 3 (33.3) | 1.23 (0.45-3.36) | .691 |
| Sulfonamides | 19 (27.5) | 3 (15.8) | 1.54 (0.11-20.71) | .744 | 4 (21) | 0.70 (0.26-1.90) | .482 |
| Carbamazepine | 6 (8.7) | 1 (16.7) | 1.91 (0.09-38.5) | .673 | 3 (50) | 0.86 (0.21-3.47) | .833 |
Ocular sequelae were the only long term complications reported in this study. In total, eleven patients (15.9%) presented with severe ocular scar or visual dysfunction, needing ophthalmologic follow-up, with diagnosis such as cicatrizing symblepharon, fornix foreshortening, severe dry eye, and corneal opacity. Usually, more than one diagnosis was present for each patient. Survivors with AIDS presented with better ocular outcome. One (4%) of the AIDS survivors and 10 (31.2%) of the non-AIDS survivors developed ocular sequelae, RR=.15 (p=.016). The main offending drugs were anticonvulsants, in five patients (45%), antibiotics in four patients (35.4%) and NSAIDS in two patients (18.2%).
All patients with ocular sequelae presented SCORTEN<4. Four survivors (30.7%) presented ocular sequelae after EN in up to 10% of the body surface area (SJS), while 7 survivors presented ocular sequelae after EN in more than 10% of the body surface area (SJS-TEN overlap or TEN), p=1.0).
The median length of hospitalization was of 30 (32), going from 1 to 210 days. Fifteen deaths occurred, with 3 deaths (20%) non-related to EN in AIDS patients with severe concomitant illnesses. A total of 12 (17.4%) patients died as a direct consequence of SJS-TEN. Seven patients (20%) died among the 35 who received only support treatment. Five patients (17.9%) died among the 28 that received systemic corticotherapy (SC). Six patients were treated with IV immunoglobulin (IG) therapy, none died. Among these, two patients received both SC and IG, and four patients received only IG. IG was prescribed as 1g/kg per day for 4 consecutive days. SC varied among pulse therapy with 1g of methylprednisolone for 3 days, oral prednisone 0.5-2mg/kg for 20 days, and even minimal prednisone doses such as 10mg/day for 5 days for an adult. The length of SC varied from 1 to 20 days. Distribution of treatment by age and year of admission, with SC, IG or both is shown in figure 2.
Figure 3 illustrates the great variety of clinical presentation of the cases.
Toxic Epidermal Necrolysis (TEN). A - Detachable skin portion above 30% of total body surface area. Severe involvement of mucous membranes, severe dysphagia causing sialorrhea, SCORTEN=3. B - Details of mucous involvement with severe ocular involvement. Ocular sequelae occurred, with formation of bilateral cicatrizing symblepharon and severe dry eye. C - Detail of a bulla. D - Child with TEN with thiabendazole as offending drug, with skin detachment of more than 60% percent of the total body surface area, with severe involvement of trunk, limbs and genitalia. SCORTEN=1
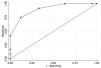
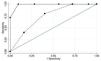
SCORTEN showed an excellent performance as death predictor with an AUC of 0.90, with 95% confidence interval (CI) ranging from .81 to .99 (Figure 4) The performance of SCORTEN was better among non-AIDS patients than in AIDS patients (p=.022), non-AIDS AUC=.99 (95% CI=.96-1.00), AIDS AUC=.74 (95% CI .53- .95),figure 5. The empirical optimal cut-off point for SCORTEN was 3.5, with 75% sensibility and 88% specificity, area under ROC curve at cut-off point of 0.81. The same optimal cut-off point was obtained non-AIDS patients, 3.5, with sensibility of 100% and specificity of 91%, area under ROC curve at cut-off point of 0.95. Among AIDS patients, the optimal cut-off point for SCORTEN was 2.5, with 80% sensibility and 60% specificity, and an area under ROC curve at cut-off point of 0.70.
Receiver Operating Characteristic (ROC) curve analysis of SCORTEN in cases admitted to a tertiary level university hospital in Brazil, from 1990 to 2014. Black: SCORTEN, AUC: 0.90, CP: 3.5 (0.75/0.88); Grey: reference line, AUC: 0.50, CP: 0.5/0.5. AUC: Area Under Curve. CP: Cut-point SCORTEN (sensitivity/specificity)
A - Receiver Operating Characteristic (ROC) curve analysis of SCORTEN in cases admitted to a tertiary level university hospital in Brazil, from 1990 to 2014. Solid: SCORTEN among patients without SIDA, AUC:0.99; CP: 3.5 (1.0/0.91). Dashes: SCORTEN among patients with AIDS, AUC:0.74; CP: 2.5 (0.8/0.6) Light grey: reference line, AUC:0.50; CP: 0.5/0.5 AIDS: Acquired Immunodeficiency Syndrome. AUC: Area Under Curve. CP: Cut-point SCORTEN (sensitivity/specificity)
Batsuji-Garin et al (2000)22 with a total of 166 patients found an AUC of .75, considering SCORTEN to be applicable to the European population. This study included 69 patients and is to date the biggest study of the kind in the American continent. The AUC obtained among all patients of .91 confirms that SCORTEN is an excellent lethality predictor in the Brazilian population. Although smaller (.74), the AUC obtained among the AIDS patients was high enough for the SCORTEN to be considered reliable in this population.
This study was conducted in a tertiary level university hospital, in which, in admissions of high complexity cases, the laboratorial parameters needed for SCORTEN calculation are performed as routine (arterial blood gas test, renal function, and serum glucose). The authors agree that, in all EN cases, the patient should ideally be admitted to an isolation hospital bed of a tertiary level hospital for high complexity support, until stabilization of the condition for hospital discharge. Maybe the hospitalization in a university tertiary level hospital, which are habituated to the management of high complexity cases, might be the cause for the slightly better global prognosis than the one predicted by SCORTEN. As seen on figure 1, from 1990 to 1998, there was a tendency to prescribe SC. After positive results of the Miami study published in 2004, the use of IG was implemented with fixed doses of 1g/kg/day for 4 consecutive days (Figures 1 and 2).10 In contrast to this, the prescribed doses of SC varied greatly during the period observed, without any standardization. One of the limitations of this study was that data were collected since a period when the calculation of SCORTEN on the first five days of admittance was not yet instituted. Therefore, many of the patients admitted on the 90’s had only one dosage of venous gases on admission, which was used as the only dosage of bicarbonate. On the other hand, even in the 90’s, all critical patients, including those in need of mechanical ventilation or with elevated respiratory rates, were monitored with sequential bicarbonate measurements, providing even more precise data.
Unfortunately, SCORTEN was not assessed routinely at the hospital of this study until 2007, when Wambier 223 This prompted a review of the approach on EN patients and altered internal procedures so as to analyze the prognosis according to SCORTEN before starting immunotherapy with IG or SC, reserving this therapy for patients with SCORTEN>2. Patients with AIDS usually received higher doses of corticoids in pulse therapy, for they were admitted to another sector of the hospital, of intensive care for AIDS patients.
According to the optimal cut-off point obtained by the ROC analysis regarding SCORTEN, of 2.5 for AIDS and 3.5 for non-AIDS and overall, to the endpoint of death related to EN, the following cut-offs for clinical decision of prescribing immunossupressive treatments could be used, SCORTEN>3, or, for a safer option, SCORTEN>2. The SCORTEN scores of highest probability of lethality in our data were 5, 6 and 7, with 100% lethality rate.
All patients with HIV included in this studied fulfilled criteria to AIDS diagnosis, either by AIDS-defining conditions or CD4 count, and were classified as AIDS C2 and AIDS C3. HIV-positive patients without AIDS were not studied because there were none in the period.
ConclusionBased on the data from this study, SCORTEN is a valid predictor of mortality in the Brazilian population, including patients with AIDS. The routine calculation of SCORTEN in these patients is recommended to help guiding treatment decision, especially in the decision of prescribing treatments such as SC pulse therapy or IVIG. Prospective, randomized trials are needed to compare the efficacy of such treatment modalities in EN.
Financial support: None.
Conflict of interest: None.