The oncogenic role of high-risk HPV in anogenital, head and neck, and cervical cancer is well recognized, but not in skin cancer in the general population. Some authors have demonstrated their appearance mainly on the hands and feet, particularly in the area of the nail bed, which could be due to contamination with HPV types from anogenital regions. Here, we describe a case of genital HPV associated with SCC on the nose tip in an immunocompetent young man, which was confirmed by histopathological findings and in situ hybridization. The importance of this report is to highlight the potential role of HPV in the etiology of skin cancer in an immunocompetent individual.
In the past decade, there has been a remarkable advance in our understanding of the natural history of human papillomavirus (HPV) infection and its role in the development of cervical and other anogenital cancers. Although the role of HPV in skin carcinogenesis has been well established in immunocompromised individuals, its association with cutaneous cancers in immunocompetent individuals remains a matter of much debate.1–4
HPV belongs to the Papillomaviridae family, which contains approximately 200 different HPVs types that can be found in five different genera: alpha, beta, gamma, mu, and nu.1,2 The mucosal HPV types, in which the oncogenic HPV types 16 and 18 are associated with the development of more than 70% of cervical carcinomas throughout the world, belong to the alpha genera. 1 The incidence of cervical cancer is still high all over the world, despite advances in treatment as well as in prophylaxis with vaccines.4
The oncogenic role of HPV is well recognized both in cervical cancer and in squamous cell carcinoma (SCC) of the anogenital and head and neck areas, which are usually associated with high-risk HPV types such as HPVs 16, 18, 31, 33, 35, 39, 45, 51, 52, 56 and 58.1,3
Although the role of HPV in skin carcinogenesis has been clearly demonstrated in patients with epidermodysplasia verruciformis (EV), its association with tumor formation, specially SCC, in the general population is not well defined, as most of the studies have yielded conflicting results. 4–8
Regarding the development of cutaneous tumors associated with high-risk genital HPV types in immunocompetent individuals, some authors have demonstrated their appearance mainly on the hands and feet, particularly in the area of the nail bed, which could be due to contamination with HPV types from anogenital regions. 3
The presence of mucosal HPV types in skin cancers localized in different regions of the body is extremely rare in immunocompetent individuals. Here, we describe a case of genital HPV associated with SCC on the nose tip in an immunocompetent young man.
Case ReportA 25-year-old Caucasian male, with no previous medical problems, presented with brown verrucous papules on the penis (Figure 1). He reported that the lesions had developed over the past year. Laboratory tests for syphilis and HIV infection were negative. The clinical and histopathologic diagnosis was condylomata acuminata. Hybridization in situ was performed using the GenPoint Catalyzed Signal Amplification System (DAKO, Carpentaria, CA)16 for high-risk (HR)-HPV (types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68; code Y1443) and low-risk (LR)-HPV (types 6 and 11) according to the manufacturer’s protocols. ISH confirmed the presence of genital high-risk HPV types.
The patient was treated with 50% trichloroacetic acid and cryotherapy every 15 days during two months and topical imiquimod 5% cream on alternate days afterwards. During the treatment, the patient developed an asymptomatic ulcerated and erythematous infiltrated plaque covered by a hemorrhagic crust measuring 0.3 cm on the nasal tip (Figure 2).
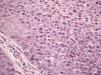
Histopathology of the nose plaque revealed Bowenoid squamous cell carcinoma and the in situ hybridization was positive for high-risk HPV types (Figures 3-6).
DiscussionBeyond the genital area, HPVs associated with cutaneous SCC are usually seen in patients with epidermodysplasia verruciformis (EV) and immunocompromised patients, e.g. organ transplant recipients (OTRs) and HIV patients.2–5 Most of these SCCs are associated with HPV related to EV (EV-HPVs).1,5,8 In immunocompetent patients, the cutaneous malignancies associated with HPV beyond the anogenital region usually occur on the periungual or subungual areas, and are associated with high-risk genital HPVs, predominantly HPV16.3 HPV related to SCC localized on the nose, as we present here, appears to be extremely rare. We did not find any description in the literature of cutaneous SCC associated with oncogenic genital HPV on the nose tip in immunocompetent individuals.
High-risk HPVs are usually associated with lesions on mucosal surfaces and are the most common subtype associated with SCC of the head and neck, including oral cancers, which suggests genital-digital and genital-oral viral spread.3 This could explain the HPV transmission path from the genital area to the patient’s nose.
Early detection of HPV induced lesions is important in order to prevent the development of cancer. The best way to diagnose an HPV infection is to confirm the presence of HPV DNA in the lesion by hybridization or PCR. The latter is expensive and is not available as a diagnostic tool in developing countries.9,10 In our case, we did not have access to PCR for HPV typing.
In summary, the importance of this report is to highlight the potential role of HPV in the etiology of skin cancer in an unexpected location in an immunocompetent individual.
Financial support: None.
Conflict of interest: None.