Dear Editor,
Warfarin-induced cutaneous necrosis is a rare complication of anticoagulant therapy with prevalence between 0.01 and 0.1%, associated to elevated morbimortality.1 It occurs almost exclusively in patients with venous thrombosis and pulmonary embolism between the 1st and the 10th day after initiation of the anticoagulation. It has been associated to the deficiency of protein C and, more rarely, to the deficiency of protein S.2
We describe the case of a man with protein S deficiency, who presented with warfarin-induced cutaneous necrosis during treatment for deep venous thrombosis.
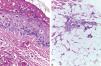
A 40-year-old man was admitted due to painful cutaneous lesions on the flanks, left thigh and left hand. His past medical history included deep venous thrombosis of the left lower limb one year back, when warfarin was prescribed. At the time, the medication was commenced along with enoxaparin. After eight months using warfarin, the patient stopped the medication on his own. Two weeks before being admitted, he noticed swelling of the right lower limb and restarted the medication without previous medical assessment and without associating a low-molecular weight heparin. Four days after restarting the medication, he noticed the appearance of the cutaneous lesions. On physical examination, he had ecchymoses on the dorsum of the left hand, flanks, lateral and anterior areas of the left thigh, that evolved with necrosis and eschar formation (Figures 1 and 2). Histopathology of the lesions demonstrated thrombosis, involving small-caliber vessels in the dermis, associated to focal epidermal necrosis (Figure 3). Doppler ultrasound of the right lower limb confirmed thrombosis. During admission, warfarin was discontinued and low-molecular weight heparin was prescribed. Thrombophilia screen revealed protein S deficiency (15% activity, normal range: 70 to 123%), normal levels of protein C and antithrombin and negative autoantibodies. The patient was discharged with low-molecular weight heparin, with gradual improvement of the cutaneous lesions. Subsequently, warfarin was reintroduced, still while using low-molecular weight heparin, with the dose increased gradually and with no appearance of new lesions.
Tissue necrosis induced by warfarin occurs more frequently in obese women, with an average age of 50 years.3 The clinical picture is usually associated to the administration of high anticoagulant doses, and the patients most susceptible to this complication are those with positive lupus anticoagulant, protein C and S, antithrombin and factor VII deficient.1
Protein S deficiency can be congenital or acquired. In the congenital form, it is determined by mutations in the gene PROS1 (3q11-q11.2), with autosomal dominant inheritance. The prevalence of partial congenital deficiency (heterozygous individuals) is estimated between 0.12 to 0.21% of the general population. The individuals with severe deficiency (homozygous) manifest the disease within the first days of life.4 Heterozygous individuals are usually asymptomatic until adulthood, what is possibly the case of the reported patient.
The pathogenesis of the warfarin-induced cutaneous necrosis is due to the pro-coagulant effects that the medication may show in the first days of use. This phenomenon occurs because the natural anticoagulant proteins C and S and factor VII, with a short half-life, have a faster decrease of their concentration than the other factors involved in pro-coagulation (factors II, IX and X), with a half-life between 20 to 60 hours. This transitory pro-coagulant/anticoagulant imbalance is exacerbated in protein C or S deficiency, leading to a hypercoagulability state with thrombotic occlusion of the microvasculature, leading to the cutaneous lesions.3
Most necrotic lesions appear in areas with abundant subcutaneous tissue. The initial lesion is a well-defined, painful erythematous macule that progresses to ecchymosis and then to necrotic tissue.5 The diagnosis is clinical, and histopathology can be helpful in confirming the diagnosis.3
Once cutaneous necrosis is diagnosed, treatment with heparin should be initiated, along with vitamin K to restore the levels of proteins C and S. The treatment includes discontinuation of warfarin; however, this procedure has not been changing the outcome.1 Good results are obtained with the cautious reintroduction of low-dose warfarin associated to anticoagulation with heparin. It is essential to know the background for the continuity of the therapy, with dosage of protein C and S, fibrinogen, fibrin degradation products levels and investigation of causes of vasculitis.3
We highlight that the medical team should be attentive to the subtlest sign or risk factor associated to this syndrome to commence treatment as quickly as possible. Even though it is not usually a life-threatening condition, the inability of early recognition and treatment can lead to sequelae that impair the patients’ quality of life.5
Financial support: None.
Conflict of Interests: None.