Dear editor,
Segmental vitiligo (SV) and localized scleroderma (LE) are characterized by localized cutaneous lesions, with a primarily autoimmune etiology. Cleft lip constitutes a congenital anomaly that is usually solitary, but can be associated with several syndromes. We report the case of a patient with left-sided cleft lip at birth, left periorbital segmental vitiligo at 6 years old, and scleroderma en coup de sabre (SCS) on the left hemiface at 22 years old.
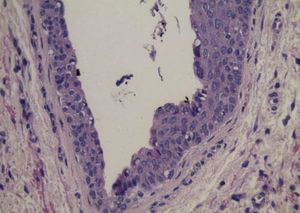
A female patient presents a linear scleroatrophic lesion located on the left forehead, compatible with SCS, by the age of 22. She presents a history of left-sided cleft lip at birth and SV on the left periorbital region, with poliosis of eyebrows and eyelashes, which began at 6 years old and stabilized at the same age (Figures 1 and 2). There is a discrete asymmetry between the hemifaces, without signs of subcutaneous, muscular, or bone atrophy beyond that presented in the SCS area. There is also a report of morphea on the upper back, with probable onset at 3 years old, currently with improvement in the sclerosis condition and histological aspect that is suggestive of post-inflammatory alterations. Other comorbidities were denied, as were allergies. There is a positive family history for vitiligo. Formal clinical and laboratorial evaluation excluded other autoimmune diseases. She underwent 31 narrow-band UVB phototherapy sessions, by the age of 18, with satisfactory cutaneous repigmentation in the SV area. Residual poliosis was also resistant to topical treatment with 0.03% bimatoprost.
The association between vitiligo and scleroderma is historically observed and described in the literature, in an attempt to find a link between these two conditions. Vitiligo is characterized by cutaneous and mucous depigmentation due to selective loss of epidermal melanocytes.1 When asymmetric, with a typical unilateral distribution, it is called SV, which usually presents a rapidly progressive but limited depigmentation, with poliosis in 50% of the cases and a greater possibility of stable repigmentation,1 as occurred in this patient. Recent evidence supports that common vitiligo and SV represent variations of the same pathological spectrum, and that the SV localized pattern is due to an autoimmune attack against a mosaic localized area.1
LS is also attributed to autoimmunity, whereby increasing collagen density leads to cutaneous sclerosis, in the absence of involvement of internal organs, acrosclerosis and Raynaud's phenomenon.2 LS that affects the skin of the frontoparietal region, often resembling a stroke from a sword, is called en coup de sabre; over time, it may lead to hemifacial atrophy.2
Although descriptions of the exact pathogenesis of SV and SL are still unknown, the above cited hypotheses are the most widespread and accepted. Few reports about the association of these two entities are found in the literature, suggesting a likely but still undefined common pathophysiology.3 Nowadays, the theory that both diseases may result from genetic mosaicism, with mutations in some ectodermal cells during the embryonic period, is accepted.1,2 In these cases, the condition develops when cells resulting from mosaicism are exposed to a yet unknown trigger, which may explain the localized character observed in these diseases.1,2
Cleft lip is a genetic anomaly that may be determined by genetic, environmental or developmental factors, and it constitutes one of the most common congenital malformations.4 This alteration in craniofacial morphogenesis occurs alone or in association with several syndromes and different embryologic signaling.4 The genetic component was partially elucidated recently, with demonstration of antagonistic signaling between the hedgehog pathway, enhanced in these patients, and the regulatory pathways WNT and p63/IRF6, which are less active, thus altering the process of facial fusion. 4 Interestingly, WNT signaling is also involved in melanocyte differentiation, with decreased expression and activation in depigmented skin from vitiligo.5
In the present report, SV, SCS and cleft lip manifestations on the same hemiface were considered atypical. This clinical situation reinforces the possible connection of these conditions to embryological cell division phenomena, highlighting mosaicism. This hypothesis can explain both the alterations in cell migration, causing cleft lip, and the alterations in some epidermal cells, which become more susceptible to localized autoimmune attacks; they may also be more likely to manifest vitiligo or scleroderma after exposure to undetermined triggers. We emphasize the hypothesis of mosaicism involvement in autoimmune dermatological diseases, which manifest in localized forms, such as scleroderma and vitiligo.