Molluscum contagiosum (MC), an infectious dermatosis caused by a virus of the Poxviridae family,1 mainly affects children, with transmission occurring through direct contact.2 It presents as 2 to 3 mm, rounded, pink, or normochromic papules, with central umbilication and a plug of caseous material.3
Although considered a self-limited disease, its treatment alleviates discomfort, and prevents infectious complications, transmission, and self-inoculation,3 refraining social marginalization of the patient and parental anxiety.
There are several types of therapy for MC2–4 but many of these methods can generate uncomfortable effects that make adherence difficult, leading to therapeutic failure, anxiety and psychological trauma for children and families.4 A widely studied method is a 5% potassium hydroxide (KOH) solution, which, despite being effective, causes uncomfortable side effects, such as pain and dyschromia.5 Therefore, it is necessary to search for other treatment options that may bring more comfort and adherence to therapy. A promising option is hydrogen peroxide (H2O2). It has antimicrobial action through the oxidation of viral molecules, damaging their DNA and leading to cytotoxicity,6 but without major damage to adjacent tissue. Thus, its adverse effects are generally mild.7 However, there is still a scarcity of studies demonstrating its real efficacy and safety.8
Accordingly, this study evaluated the efficacy and safety of using H2O2 1% cream as MC treatment in pediatric patients. And, it was comparared with KOH 5% solution, through a double-blind, randomized, placebo-controlled pilot study with 30 patients with MC, aged 2 to 16 years, who had had no treatment for the disease in the previous six months, randomly allocated into three treatment groups following the order of arrival. Group A was submitted to treatment with H2O2 1% cream; Group B, treatment with KOH 5% solution; Group C, treatment with Lanette cream (placebo), all applied twice a day, continuously used until the lesions became irritated. The participants were evaluated every 4 weeks for three months through photographic records and clinical evaluation by a dermatologist blinded to the intervention, regarding the number of lesions, their reduction, and side effects. Parents perception was also recorded throughout a specific questionnaire. Of the 30 patients, seven did not complete the study (five due to poor adherence to treatment; one due to loss of follow-up; and one due to an adverse effect of KOH), leaving 23 individuals - eight in Group A, seven in Group B and eight in Group C.
Regarding the percentage reduction of lesions (Fig. 1), in the 4th week, there was a greater reduction of 50% of lesions in almost 40% of the patients in Group A, close to Group B (42.9%; p = 1) and higher than Group C (25%; p = 1). In the 12th week, this reduction reached 85% of the patients in Group A, lower than in Group B (100%), but higher than in Group C (62.5%; p = 1).
The absolute reduction in the number of total lesions (Fig. 2), considering the sum of all patients, was 20.7% in Group A in the 4th week, lower than that obtained in Group B (41.2%; p = 0.265). Both Group A and Group B showed higher values than the placebo group, which on the other hand showed an increase in the number of lesions during this period. In the 12th week, 73.2% of the lesions had resolved in Group A (p = 0.034), lower than the 98.4% reduction seen in Group B (p = 0.034), but higher than in Group C (45.5%; p = 0.034).
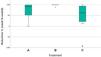
It was also observed that Group A showed greater variability in results between patients, while Group B showed almost no dispersion. Although Group C also had cases of improvement, there were cases of worsening of the condition (Fig. 3).
Regarding parents perception of side effects, from the 4th to 12th week (p = 1, p = 1, p = 0.846), 50% of the patients in Group A experienced some adverse event. In Group B, 70% of the patients experienced adverse effects in the 4th week, 42.9% in the 8th week and more than 80% in the 12th week (p = 1, p = 1, p = 0.846, respectively). There were also reports of adverse effects in Group C, 37.5%, 25% and 75% in weeks 4, 8 and 12, respectively, which can be attributed to symptoms of the natural evolution of the disease.3
Of the reported side effects, erythema was present in 37.5% of the patients in Group A in the 4th week, similar to what was found in Group C (37.5%; p = 1) and lower than that in Group B (57.1%; p = 1). In the 12th week, Group A showed more erythema when compared to the other groups (A: 37.5%; B: 14.3%; C: 12.5%; p = 1).
As for crusts, they were present in 25% of the patients in Group A in the 4th week and absent in the 8th and 12th weeks, while in Group B, they were present in 14.4% throughout all weeks, close to the values in Group C (13%; p = 1).
As for erosions/ulcers, Groups A and C did not show them in any of the evaluations, whereas 14.3% of all patients in Group B had these signals in the 12th week.
Pruritus was more prevalent in Group A compared to the two other groups in all weeks, affecting 25% of children in the 12th week. Group B, on the other hand, did not report pruritus, unlike other studies, in which this symptom is a common finding.8
Burning/pain sensation was present in 12.5% of individuals in Group A in all weeks, the same as in Group C (12.5%). In Group B, this value was almost four times higher in the 4th week (57.1%; p = 0.357); and reached 71.4% of the patients in the 12th week (p = 0.122).
In Group A, 25% of the children had dyschromia in the 12th week, lower than what was seen in Group C (37.5%, p = 1) and also Group B, which had 71.4% in the 4th week (p = 0.021), with persistence of the condition in almost half of the patients in the 12th week (42.9%; p = 1).
It can be concluded that the use of H2O2 showed a tendency towards superior efficacy in relation to the placebo, but still lower than that of KOH. However, it seems to be a promising therapy due to its safety and lower incidence of side effects such as burning sensation, pain and dyschromia. Due to these findings, it may be a good option for younger children, with more sensitive skin and intolerant to the adverse manifestations caused by KOH. As this is a pilot study with a small sample, it did not obtain the necessary statistical significance to allow a conclusion on the real effectiveness of H2O2, requiring further larger sample studies to guarantee statistically significant efficacy and safety results.
Financial supportWe had financial support from FUNADERM (Fundo de Apoio à Dermatologia).
Authors’ contributionsElinah Narumi Inoue: Data collection, analysis and interpretation of data; drafting and editing of the manuscript; collection, analysis and interpretation of data; critical review of the literature.
Felipe de Paula Saboia: Data collection.
Amanda Hertz: Data collection.
Marcia Olandoski: Statistical analysis.
Dâmia Kuster Kaminski Arida: Design and planning of the study; data collection, or analysis and interpretation of data; drafting and editing of the manuscript or critical review of important intellectual content; collection, analysis and interpretation of data; effective participation in research orientation; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; approval of the final version of the manuscript.
Conflicts of interestNone declared.
Study conducted at the Pediatric Dermatology Outpatient Clinic, Department of Dermatology, Hospital Universitário Evangélico Mackenzie, Curitiba, PR, Brazil.