This study describes a case of a 19-year-old patient with seven asymptomatic lesions on the chest, measuring between 0.5 to 1cm in diameter, with no history of trauma in the region. The immunohistochemical evaluation was positive for vimentin and smooth muscle actin, determining Dermatomyofibroma as definitive diagnosis. Dermatomyofibroma is a benign skin tumor, with a myofibroblastic origin, prevalent in young women. It usually presents as a single lesion, with very few reports of multiple lesions.
Dermatomyofibroma is a relatively rare benign mesenchymal cutaneous tumor of myofibroblastic origin.1
Clinically, it presents as an asymptomatic plaque or nodule, usually measuring between 1 cm and 5cm in diameter. However, there are reports of larger dermatomyofibromas.2,3 Its coloration can vary from skin-color to red-brown. It occurs preferentially in young women and pre-pubertal children.4,5
The most commonly affected areas of the body are shoulder, axilla, neck and upper trunk.6 It presents as a single lesion; cases with multiple lesions are rare.2
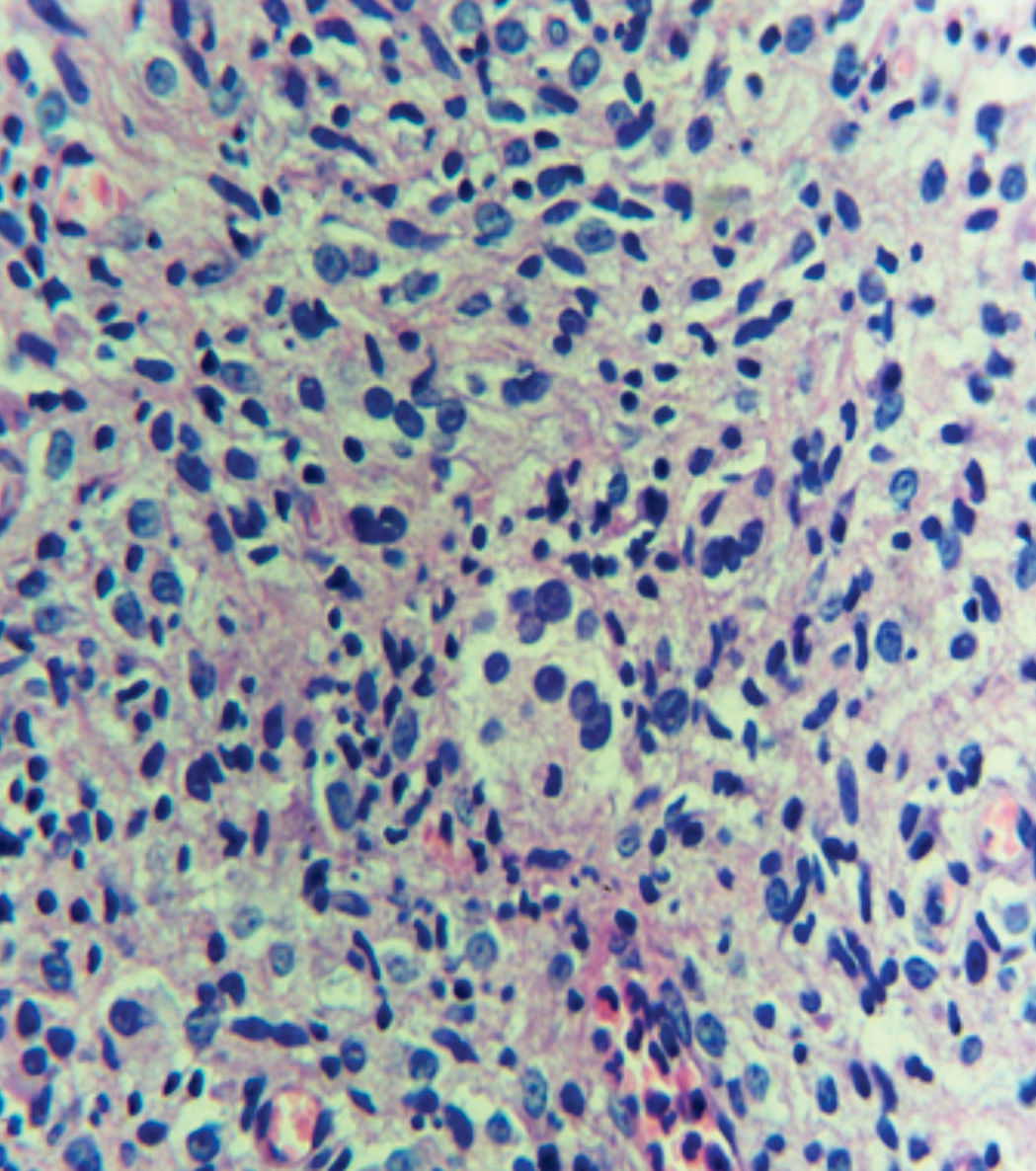
Case ReportA female, 19-year-old patient, student, presented with seven asymptomatic, firm lesions on the upper trunk (pre-sternal region), measuring between 0.5 cm and 1 cm in diameter, with a course of approximately 20 months. There was no history of trauma in the area. She reported going to other services previously, and having an incisional biopsy three months back of the lesion closest to the right breast. The diagnosis then was of a foreign body-type granulomatous reaction. However, the history and clinical examination of the patient were not consistent with the proposed diagnosis, and in the biopsy slide no etiological agent or other possible cause was identified (Figure 1). Therefore, we opted to perform an excisional biopsy of the upper right lesion (Figure 2).
Histopathology revealed a proliferation of elongated fibroblasts, with oval-shaped and vesicular nuclei, very few with vacuoles, and cells arranged in parallel bundles, evidencing thin, mature interspersed collagen and foci of surrounding lymphocytic inflammatory infiltrate. There were no histological signs of malignancy or inflammatory process. The diagnosis was nodular cutaneous fibromatosis (Figure 3).
In view of many diagnostic hypotheses, such as dermal fibromatosis, nodular fasciitis, granuloma annulare, dermatofibroma, among others, we requested immunohistochemistry evaluation. At the time, to confirm the previous diagnosis, we requested a second histopathology.
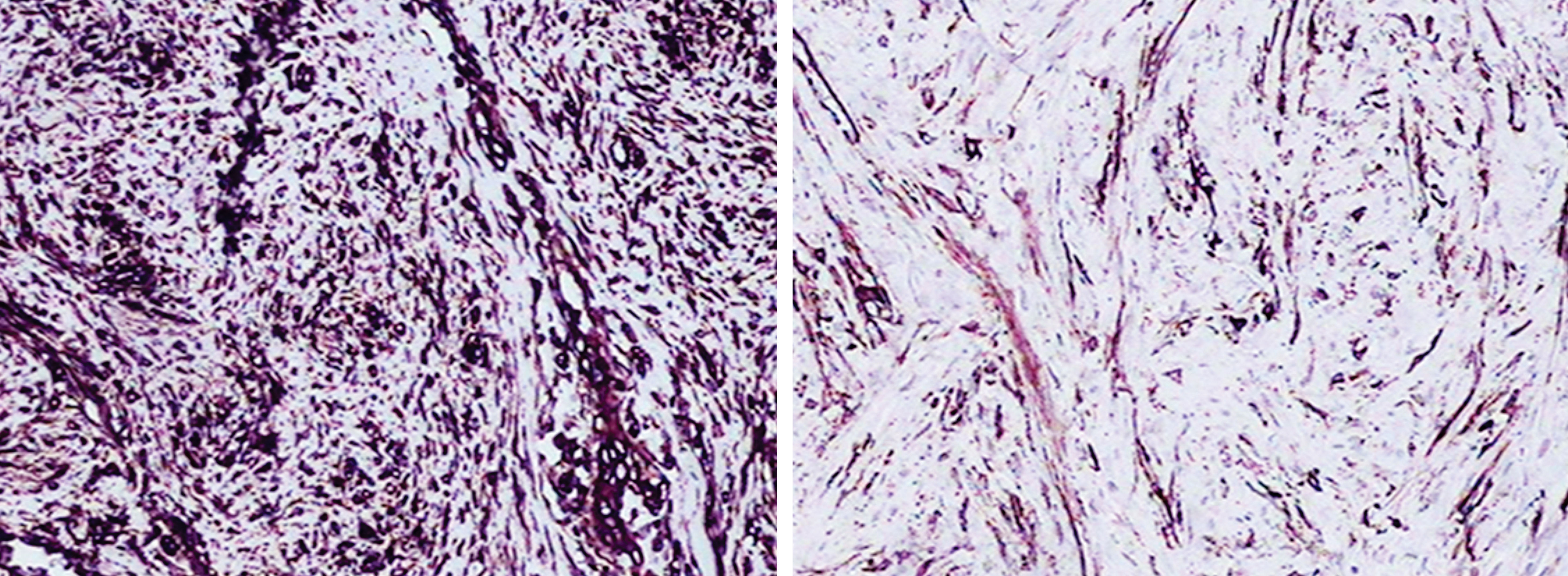
Immunohistochemistry then revealed focally positive smooth muscle actin, positive vimentin and negative cytokeratin, desmin, beta catenin, CD34, calponin and CD68. Histopathology showed spindle cells with no atypia and no mitotic figures (Figure 4). We concluded that the finding was consistent with benign fibroblastic/myofibroblastic proliferation, and the diagnosis proposed was of hypertrophic scar.
After thorough analysis of all studies performed and the correlation with clinical findings, we established the definitive of dermatomyofibroma.
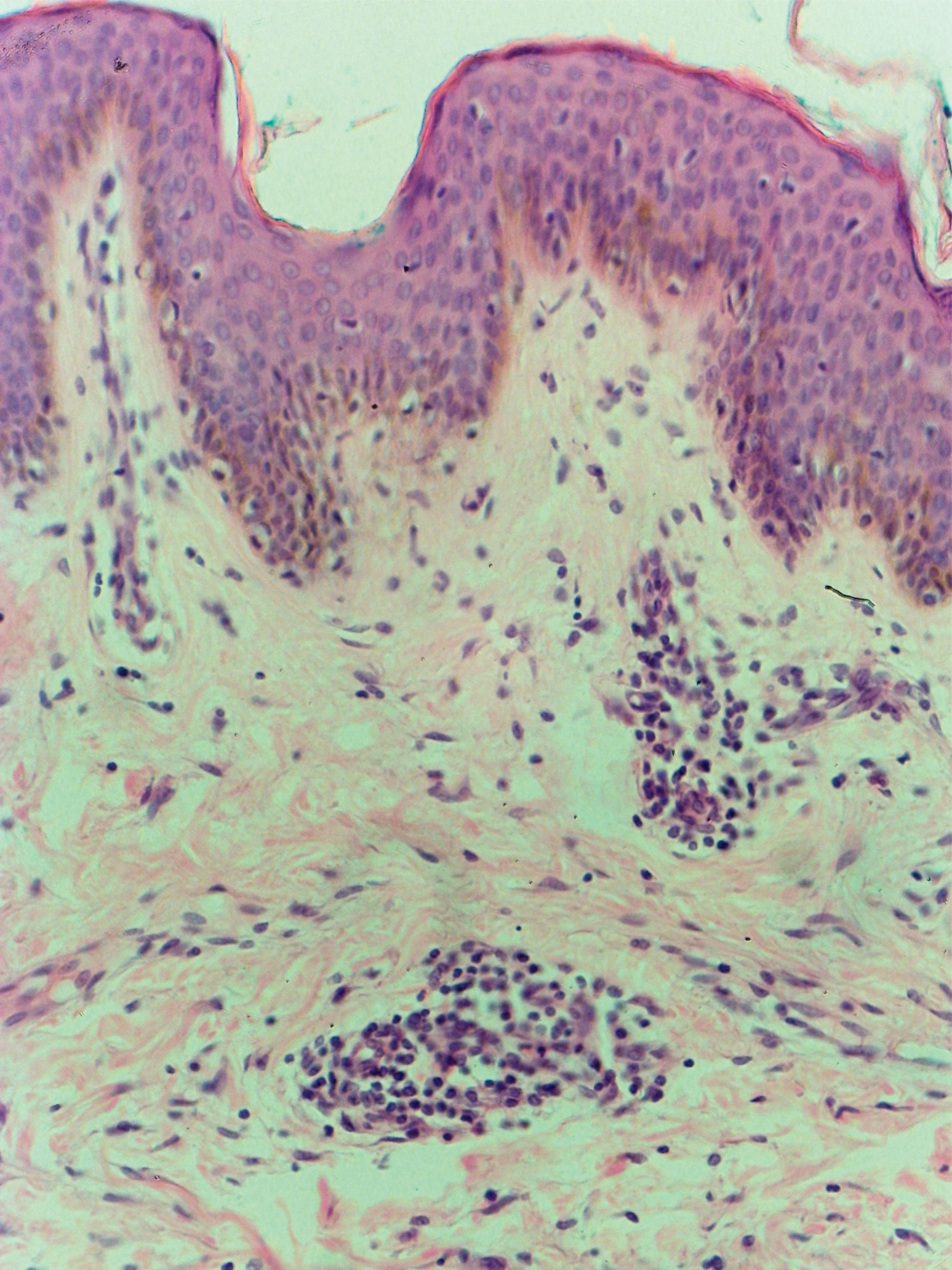
DiscussionDermatomyofibroma is a little known benign tumor and thus, many times misdiagnosed.7 Microscopically, it presents as a well-defined diffuse proliferation of spindle cells, separated by collagen fibers and located on the reticular dermis. They have wide eosinophilic cytoplasms and elongated or oval-shaped nuclei. The main features of the tumor are the orientation of the cells, parallel to the surface of the epidermis, the preservation of appendices and absence of mitoses and atypia.2,7,8
The importance in establishing the diagnosis of dermatomyofibroma resides in distinguishing it from other invasive tumors, that have different treatment and prognosis, such as dermatofibrosarcoma protuberans and piloleiomyoma.1-3,5,6 Immunohistochemistry is fundamental to eliminate doubts and confirm the diagnosis, as happened in this case, where the negative CD34 and desmin ruled out both conditions, respectively.1-3,5,8
Dermatomyofibroma can also be mistaken by a hypertrophic scar. Some authors say that the differentiation between them can be done by the presence of elastic fibers, that are preserved in dermatomyofibroma1,2,6,9 and abnormal or absent in hypertrophic scars.1-3,6 However, for Ferreira and D’Assumpção, elastic fibers are almost absent in keloids, but can be found in hypertrophic scars, what can make differentiation difficult.10 Moreover, other differentiating factors must be considered, such as the course of the lesion, the etiology and clinical aspect. Dermatomyofibroma is not caused by trauma in the affected area and grows slowly but steadily, as opposed to hypertrophic scar, that appears after an injury and tends to regress spontaneously sometime after the initial trauma.2,9,10 Clinically, hypertrophic scars are raised, firm and restricted to the margins of the original lesion,2,10 whereas dermatomyofibroma usually presents as a small lesion, many times more palpable than visible.2,9
Thus, for correctly diagnosing this condition, besides histopathology and immunohistochemistry, it is important to conduct a good interview and also a detailed physical examination, in which palpation becomes a valuable tool.
In this case, besides performing all the above-mentioned procedures, we requested photos of the patient’s daily life between a year before the appearance of the lesions and the moment of the excisional biopsy, in order to assess the course of the lesions. In the photos, we observed that the fastest speed of growth occurred in the first 6 months after their appearance, when they changed from almost invisible dots into visible lesions. After this period, there was a reduction in growth speed.
Multiple dermatomyofibromas are extremely rare, with few reports worldwide.2 In this case, besides the rarity of the condition, the multiple lesions made the diagnosis difficult, requiring in depth studies in order to make the distinction between other fibroblastic skin entities relevant to the affected site.
The treatment of choice dermatomyofibroma is surgical excision, with an excellent prognosis.1-3,5,6,8,9 However, in our patient, surgical excision resulted in keloid scarring, followed by pain, pruritus and considerable cosmetic disfigurement (Figure 5). Therefore, we opted to follow the other lesions clinically as an alternative to surgical excision, temporarily avoiding a worse cosmetic outcome in the area.
We conclude that, due to the rarity of the condition, especially in the multiple form and due to the diagnostic difficulty, the reported case in of fundamental importance for the dermatologic clinical practice, since dermatomyofibroma can be easily misdiagnosed, the reason why we considered its description relevant.
Financial support: None.
Conflict of interest: None.