Background: Non-melanoma skin cancer accounts for a third of all malignancies registered in Brazil, with squamous cell carcinoma (SCC) being one of its subtypes. It develops in photo-exposed areas, affecting social habits and causing negative influence on quality of life (QoL).
Objectives: To evaluate QoL in patients with primary cutaneous SCC.
Methods: A cross-sectional study was performed in patients with clinical diagnosis of SCC, corroborated by dermoscopy and confirmed by histopathology; prior to resection of the tumor using the double-blade scalpel technique, a questionnaire on the Dermatology Life Quality Index (DLQI) was applied.
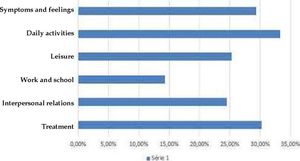
Results: Among the 46 evaluated patients, mean age was 67.1 ± 16.0 years, with a predominance of males, low educational level and socioeconomic status, Fitzpatrick II phototype, history of outdoor work, and tumor location in exposed photo areas. Mean DLQI was 4.02 ± 0.63, and in the categorization, 11 (23.9%) had a moderate to severe negative effect on QoL. The skin tumor had a negative impact on daily activities (33% of cases), treatment effects (30%), and symptoms and feelings (29%).
Study limitations: There is no gold standard instrument for assessing QoL in dermatological patients.
Conclusion: In the study sample, one-fourth of patients with SCC had a moderate to severe negative effect on quality of life.
Skin cancer, currently the most frequent neoplasia in Brazil, is classified in the melanoma and non-melanoma subtypes, the latter accounting for one-third of all malignant tumors recorded in the country. The National Cancer Institute (INCa) has estimated 85,170 new cases in men and 80,410 in women in 2018, based on national epidemiological studies indicating a 29.0% increase in males and 32.8% in females in the occurrence of non-melanoma skin tumors.1,2 When assessing non-melanoma tumors, 75% are basal cell carcinoma (BCC), 20%, squamous cell carcinoma (SCC), and 5% other subtypes.
SCC develops from pre-neoplastic alterations, including keratosis and actinic cheilitis, and diagnosis is based on clinical characteristics and complemented with dermoscopy, but histological confirmation is necessary to establish the prognosis and adequate management of the lesion.3–5 The main risk factor for the development of this neoplasia is exposure to ultraviolet (UV) rays, but other factors such as ionizing radiation, chronic inflammation, atrophic diseases (post-burn and post-irradiation scar), immunosuppression, HPV infection (types 16 and 18), chemical agents, smoking, and alcohol use have also been reported.4–6 Treatment includes excisional biopsy with histopathological control of margins.7,8
The improvement in health-related quality of life (HRQoL), defined as perception of the effects of the disease and the treatment in its physical, psychological, and social aspects, is an important treatment target in skin cancer, since the treatment can cause functional and aesthetic limitations.9,10 The diagnosis per se and the possibility of developing a second primary skin cancer, even after the cure of initial tumor, can cause anxiety.11
Based on this premise, we proposed a study to assess QoL in patients with diagnosis of primary cutaneous SCC prior to resection of the tumor by double-bladed scalpel (DBS), treated at a public teaching hospital in the South of Brazil.
MethodsThis was an observational, cross-sectional epidemiological study with an analytical component, conducted at the Plastic Surgery and Burn Clinic in a public teaching hospital in a university in the South of Brazil from March to December 2016. We initially assessed 54 patients ages 18 years and older, consecutively, with clinical diagnosis of SCC, screened by clinical dermatologists using dermoscopy as an ancillary tool. Anatomical pathological examination was performed in paraffin at the Pathology Service in this same hospital, which confirmed the neoplasia in 50 cases.
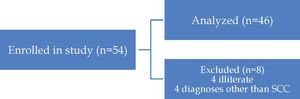
Demographic, clinical-surgical, and lifestyle data were collected before the surgical procedure, as well as application of the quality of life questionnaire.12 At this stage, four more patients were excluded because they were unable to complete the questionnaire, leaving a total sample of 46 patients.
The patients’ demographic and clinical-surgical characteristics were assessed, and the anatomical pathological diagnosis and quality of life score were defined for the lesion, the latter measured by the Dermatology Life Quality Index (DLQI), a generic instrument developed for diseases of the skin and connective tissue, with translation and cross-cultural validation in Brazilian Portuguese.12,13 The score, shown in chart 1, consists of ten questions, grouped in six domains (symptoms and feelings, daily activities, leisure, work and school, interpersonal relations, and treatment). On the ‘treatment’ item, the answers to question 10 considered surgical and non-surgical treatments of the target skin lesions, since patients were initially treated in Basic Health Units (Chart 1). The data were keyed into a computerized teledermatology system, and patients were then treated by this hospital’s surgical team in the South of Brazil. Most of the patients were attending periodic consultations and assessments or were using topical treatments for the skin lesions, and were thus considered in treatment. Each question is scored from 0 (nothing/ not relevant) to three (extremely), on a Likert scale. The values for this index vary from 0 to 30, in which zero (0) indicates absence of effects on life and 30 indicates a very large effect. The final score is classified as: 0-1=no effect; 2-5=small; 6-10=moderate; 11-20=serious; and 21-30=very serious.12 The study excluded patients with diagnosis of other subtypes of cancer, with relapsed cutaneous SCCs, in use of nonsteroidal anti-inflammatory drugs, in use of systemic corticosteroids, in use of tumor necrosis factor inhibitors (anti-TNF), with active inflammatory diseases, under 18 years of age, illiterate, and immunosuppressed individuals (such as those with primary immunodeficiency syndrome and/or renal transplant patients).
Dimensions and domains assessed by the DLQI, validated in Portuguese12
| Questions | Domains | Possible answers |
|---|---|---|
| 1. Over the last week, how itchy, sore, painful, or stinging has your skin been?2. Over the last week, how embarrassed or self-conscious have you been because of your skin? | Symptoms and feelings | 3 - Very much2 - A lot1 - A little0 - Not at all |
| 3. Over the last week, how much has your skin interfered with you going shopping or looking after your home or garden?4. Over the last week, how much has your skin influenced the clothes you wear? | Daily activities | 3 - Very much2 - A lot1 - A little0 - Not at all |
| 5. Over the last week, how much has your skin affected any social or leisure activities?6. Over the last week, how much has your skin made it difficult for you to do any sport? | Leisure | 3 - Very much2 - A lot1 - A little0 - Not at all |
| 7. Over the last week, has your skin prevented you from working or studying? “No”, over the last week how much has your skin been a problem at work or studying? | Work and school | 3 - Very much2 - A lot1 - A little0 - Not at all |
| 8. Over the last week, how much has your skin created problems with your partner or any of your close friends or relatives?9. Over the last week, how much has your skin caused any sexual difficulties? | Personal relations | 3 - Very much2 - A lot1 - A little0 - Not at all |
| 10. Over the last week, how much of a problem has the treatment for your skin been, for example, by making your home messy, or by taking up time? | Treatment | 3 - Very much2 - A lot1 - A little0 - Not at all |
DLQI: Dermatology Life Quality Index. Results with Likert score: 0-1: no effect; 2-5: small effect; 6-10: moderate effect; 11-20: serious effect and 21-30: very serious effect. Source: Finlay et al., 1994.12
The surgical procedure was performed as proposed by Schultz, which consists of marking the tumor, where tumors less than 2cm result in a margin of 10mm and those larger than 2cm in a margin of 15mm (Figure 1).14,15
A - Marking margins; B - Excision of lesion with double-bladed scalpel; C - Removal of safety margin with double-bladed scalpel; D - Separation of margins for subsequent analysis and staining; E - Specimens marked with India ink; F - Marking with nylon suture at 12:00. Protocol for surgical procedure performed in patients with squamous cell skin cancer
Source: Girschik et al, 2008.17
Statistical analysis described the continuous variables as means (standard deviation) or median (percentiles) after application of the Kolmogorov-Smirnov, Shapiro-Wilk, and Lilliefors tests of normality, and the categorical variables were described as absolute values and proportions. Measures of association were calculated by the chi-square test (x2) or Fisher’s exact test, when appropriate, and odds ratios were also obtained. Statistical significance was determined with 95% confidence intervals and p-value < 0.05. The analyses used the Statistical Package for the Social Sciences®, version 22.0 (IBM SPSS Statistics, Chicago, Illinois, USA).
The study project was approved by the university’s Institutional Review Board under number CAE - 51985215.6.0000.0121. Patients’ confirmed their voluntary participation by signing a free and informed consent form.
ResultsOf the 54 patients listed for the study, eight were excluded from the analysis (four illiterate patients and four with diagnoses other than SCC - two basosquamous carcinomas and two basal cell carcinomas) (Figure 2).
Of the 46 patients that were assessed, mean age was 67.1±16.0 years, with 31 men (67.4%), most of whom with outdoor occupations, or a total of 41 (89.1%). Of these workers, 26 (56.6% of the total) were farmers, and 58.7% were Fitzpatrick phototype II.16 The socioeconomic characteristics showed a predominance of low schooling (36 patients or 78.3% had incomplete primary schooling) and low income (38 patients or 82.6% of the sample earning up to twice the minimum wage, or about U$480/month). There was a personal history of skin cancer in 50% of the patients (23/46), and 20/46 (43.4) had a positive family history. Half of the sample had a single lesion and the other had multiple lesions. When quality of life was assessed on the basis of DLQI scores, the mean value was 4.02±0.63; in the categorization, approximately one-fourth of patients (23.98%) scored greater than five, indicating a moderate to severe negative effect on quality of life (Table 1).
Demographic and clinical characteristics of patients with diagnosis of squamous cell carcinoma (n=46)
| Variables | Values |
|---|---|
| Age (years)£ | 67.1 ± 16.0 |
| Male gender | 31(67.4%) |
| Profession | |
| Outdoor work | 41(89.1%) |
| Indoor work | 5(10.9%) |
| Skin phototype (Fitzpatrick) | |
| II | 27(58.7%) |
| III | 16(34.8%) |
| IV | 3(6.5%) |
| Schooling | |
| Incomplete primary | 36(78.3%) |
| Complete primary or more | 10(21.7%) |
| Family income | |
| Up to two times the minimum wage | 38(82.6%) |
| >2 and <6 times the minimum wage | 8(16.4%) |
| Personal history of skin cancer | 23(50.0%) |
| Family history of skin cancer | 20(43.4%) |
| Malignant lesions | |
| Single | 23(50%) |
| Multiple | 23(50%) |
The sample showed a high rate of solar exposure and low use of sunscreen. Mean exposure was 44.7±18.3 years, and 82.6% were exposed to sun from 10:00 AM and 4:00 PM. Only 26 (56.5%) individuals had ever used sunscreen (Table 2). Approximately half were smokers (54.3%) and reported alcohol consumption (43.5%). As for hats and protective clothing, 71.7% reported regular use.
Comorbidities and life habits in patients with cutaneous squamous cell carcinoma (n=46)
| Systemic arterial hypertension | 21(45.7%) |
| Diabetes mellitus | 5(10.9%) |
| Rheumatoid arthritis | 1(2.2%) |
| Psoriasis/vitiligo | 2(4.4%) |
| Smoking | 25(54.3%) |
| Pack years* | 25(20-40) |
| Alcohol abuse | 20(43.5%) |
| Solar exposure (years) | 44.7±18.3 |
| Exposure between 10:00 AM and 4:00 PM | 38(82.6%) |
| Chemical photoprotection (use of sunscreen) | 26 (56.5%) |
| Mechanical photoprotection (use of hat or long clothing) | 33(71.7%) |
Data shown in absolute numbers (percentage)*Median (P25-P75); # mean (±standard deviation)
The lesions predominated on photoexposed areas, with head and neck as the most common (52.2%), followed by upper limbs with 26.1%. Three cases (6.5%) had positive deep margins. Concerning analysis of the peripheral margins, no involvement was found with conventional anatomical pathological analysis, and one case (2.2%) was observed when we used the double-bladed scalpel technique. We thus had one false-negative result (Table 3).
Clinical/surgical and anatomical/pathological characteristics of cutaneous squamous cell carcinoma (n=46)
| Location | |
| Head and neck | 24(52.2%) |
| Upper limbs | 12(26.1%) |
| Trunk | 3(6.5%) |
| Histological subtypes | |
| In situ | 27(58.7%) |
| Invasive | 19(41.3%) |
| Differentiation by anatomical pathology | |
| Poorly differentiated | 3(6.5%) |
| Moderately differentiated | 13(28.3%) |
| Well-differentiated | 8(17.4%) |
| Layers invaded by lesion - Assessed by anatomical pathology | |
| Hypodermis | 7(15.2%) |
| Papillary dermis | 4(8.7%) |
| Reticular dermis | 7(15.2%) |
| Positive deep margins | 3(6.5%) |
| Positive peripheral margins | 1(2.2%) |
| Surgery performed | |
| Primary suture | 18(39.1%) |
| Graft | 13(28.3%) |
| Flap | 10(21.7%) |
| Second intention | 5(10.9%) |
| Duration of procedure (minutes) * | 32(10-120) |
| Data presented in absolute numbers (percentage); *Median (minimum-maximum) |
Data shown in absolute numbers (percentage)*Median (P25-P75); # mean (±standard deviation)
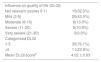
Table 4 shows the influence of lesions assessed by the DLQI score. Table 5 is the absolute distribution of the score on the answers obtained with the same quality of life questionnaire. Table 6 presents absolute numbers divided across the domains.
Patients’ characteristics in relation to quality of life measured by DLQI
| Influence on quality of life (DLQI) | |
| Not relevant (scores 0-1) | 15(32.0%) |
| Mild (2-5) | 20(43.5%) |
| Moderate (6-10) | 6(13.0%) |
| Severe (11-20) | 5(10.9%) |
| Very severe (21-30) | 0(0.0%) |
| Categorized DLQI | |
| 1-5 | 35(76.1%) |
| >5 | 11(23.9%) |
| Mean DLQI score£ | 4.02 ± 0.63 |
Source: Finlay et al, 1994.12
Mean±standard deviation; other values present in absolute numbers (percentage); DLQI - Dermatology Life Quality Index12
Dermatology Life Quality Index (DLQI): distribution of scores in patients with SCC
| Score | |||||||
|---|---|---|---|---|---|---|---|
| Number | Question | 0 | 1 | 2 | 3 | Not relevant | Not completed |
| 1 | Itching stinging/pain | 10 | 23 | 9 | 4 | - | 0 |
| 2 | Embarrassment/self-consciousness | 25 | 14 | 6 | 1 | - | 0 |
| 3 | Effect on household work | 15 | 17 | 11 | 3 | 0 | 0 |
| 4 | Effect on clothing | 15 | 20 | 7 | 4 | 0 | 0 |
| 5 | Effect on planning leisure time | 16 | 17 | 8 | 3 | 2 | 0 |
| 6 | Effect on sports | 29 | 15 | 1 | 1 | 0 | 0 |
| 7* | Effect on work | - | 18 | 5 | - | 23 | 0 |
| If “no” to question 7 (n=18) | 12 | 6 | 0 | - | - | 0 | |
| 8 | Problems in relations with others | 17 | 20 | 7 | 2 | 0 | 0 |
| 9 | Effect on love life | 23 | 19 | 3 | 1 | 0 | 0 |
| 10 | Problems resulting from treatments for skin conditions | 17 | 18 | 9 | 1 | 1 | 0 |
Source: Finlay et al, 1994.12
Distribution of quality of life scores in different domains in patients with squamous cell carcinoma
| Quality of life n (%) | ||||||
|---|---|---|---|---|---|---|
| DLQI | Symptoms and feelings | Daily activities | Leisure | Work and school | Interpersonal relations | Treatment |
| 0 | 9 (19.6%) | 13 (28.3%) | 14 (30.4%) | 36 (78.3%) | 17 (37.0%) | 17 (37.0%) |
| 1 | 12 (26.1%) | 5 (10.9%) | 9 (19.6%) | 5 (10.9%) | 4 (8.7%) | 18 (39.1%) |
| 2 | 13 (28.3%) | 13 (28.3%) | 13 (28.3%) | 0 (0.0%) | 18 (39.1%) | 9 (19.6%) |
| 3 | 8 (17.4%) | 5 (10.9%) | 6 (13.0%) | 5 (10.9%) | 3 (6.5%) | 2 (4.4%) |
| 4 | 2 (4.3%) | 5 (10.9%) | 3 (6.3%) | - | 2 (4.3%) | - |
| 5 | 1 (2.2%) | 4 (8.7%) | 1 (2.2%) | - | 1 (2.2%) | - |
| 6 | 1 (2.2%) | 1 (2.2%) | 0 (0.0%) | - | 1 (2.2%) | - |
| Total | 46(100.0%) | 46(100.0%) | 46(100.0%) | 46(100.0%) | 46 (100.0%) | 46(100.0%) |
Source: Finlay et al, 1994.12
Graph 1 describes the percentage of the tumor’s negative influence on individuals’ quality of life in each of the categories, with the highest proportion found in activities of daily living (33%), treatment-related effects (30%), and symptoms and feelings (29%).
Table 7 categorizes the sample in two groups to diagnose protective and risk factors related to DLQI. The first group included individuals that scored less than five points (little or no influence on quality of life) and the second included values greater than five points (moderate, severe, and very severe). The odds ratio was 0.88 (CI: 0.22- 3.43) when related to tumor location (p= 0.03) (Table 7).
Sociodemographic and clinical characteristics and use of protection from solar exposure according to Dermatology Life Quality Index (DLQI)
| DLQI scores | ||||
|---|---|---|---|---|
| Characteristics | Not relevant or mild | Moderate, severe, or very severe | odds ratio (95% confidence interval) | p-valueμ |
| Age (years) | ||||
| < 68 | 16 (72.7%) | 6 (27.3%) | 0.70 (IC 0.18-2.73) | 0.26 |
| >68 | 19 (79.2%) | 5 (20.8%) | ||
| Gender | ||||
| Male | 22 (71.0%) | 9 (29.0%) | 2.65 (IC 0.49-14.24) | 1.47 |
| Female | 13 (86.7%) | 2 (13.3%) | ||
| Work activities | ||||
| Outdoor | 24 (77.4%) | 7(22.6%) | 0.80 (IC 0.19-3.32) | 0.09 |
| Indoor | 11 (73.3%) | 4 (26.7%) | ||
| Fitzpatrick | ||||
| II | 19 (70.4%) | 8 (29.6%) | 0.44 (IC 0.10-1.96) | 1.21 |
| III-IV | 16 (84.2%) | 3 (15.8%) | ||
| Monthly income | ||||
| ≤ 2 minimum wages | 28 (73.7%) | 10 (26.3%) | 0.40 (0.04-3.66) | 0.65 |
| 2-6 minimum wages | 7 (87.5%) | 1 (12.5%) | ||
| Schooling | ||||
| Incomplete primary | 26 (72.2%) | 10 (27.8%) | 0.28 (IC 0.03-2.58) | 1.56 |
| ≥ complete primary | 9 (90.0%) | 1 (10.0%) | ||
| Number of lesions | ||||
| Single | 18 (78.3%) | 5 (21.7%) | 1.27 (IC 0.32-4.94) | 0.11 |
| Multiple | 17 (73.9%) | 6 (26.1%) | ||
| Smoking | ||||
| Yes | 18 (85.7%) | 3 (14.3%) | 2.82 (IC 0.64-12.44) | 1.96 |
| No | 17 (68.0%) | 8 (32.0%) | ||
| Solar exposure 10AM-4PM | ||||
| Yes | 7 (87.5%) | 1 (12.5%) | 2.50 (IC 0.27-22.93) | 0.65 |
| No | 28 (73.7%) | 10 (26.3%) | ||
| Sunscreen | ||||
| Yes | 17 (89.5%) | 2 (10.5%) | 4.25 (IC 0.80-22.5) | 3.44 |
| No | 18 (66.7%) | 9 (33.3%) | ||
| Physical photoprotection | ||||
| Yes | 10 (76.9%) | 3 (23.1%) | 1.06 (IC 0.23-4.85) | 0.007 |
| No | 25 (75.8%) | 8 (24.2%) | ||
| Tumor site | ||||
| Head\neck | 18 (75.0%) | 6 (25.0%) | 0.88 (IC 0.22-3.43) | 0.03 |
| Trunk\limbs | 17 (73.3%) | 5 (22.7%) | ||
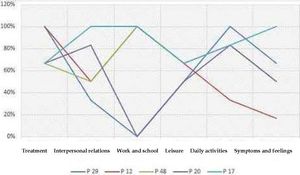
Individuals that presented severe influence on quality of life (n=5), as expressed by a very high DLQI (11-20), are shown in Graph 2, with their individual scores subdivided by domains. All of them were men who presented lesions on the face or neck and were 50 to 60 years of age.
Quality of life index in patients with very high score (11-20) in different domains and location of SCC P 17: 59 years (A), malar region, DLQI: 20; P 20: 54 A, pre-auricular region, DLQI:11; P 48: 57 A, auricular region, DLQI: 13; P 12: 53 A, pre-auricular region, DLQI: 11 and P 29: 53 A, malar region, DLQI: 12
Legend: P= patient and respective identification number, age, location of SCC, quality of life index, very high score (11 to 20)
Squamous cell carcinoma accounts for only 20% of non-melanoma skin tumors but is responsible for the majority of the fatal cases.17 This neoplasm generally occurs in older men after chronic exposure to solar radiation, which may be due to the higher male participation in activities with cumulative exposure to UV rays. Approximately 97% of cases are associated with malignant progression of an actinic keratosis.3,8,9 However, it has increasingly affected the younger population, which may be explained by early detection, increasing use of tanning salons, ozone layer depletion, and increase in high-risk groups (organ transplant recipients and patients with bullous epidermolysis).18,19 The majority of our patients were males (67.4%) and worked outdoors (89.1%).6
Most of the patients with SCC had light skin (Fitzpatrick type II), low schooling (69.6% had not finished primary school), and smoked (53.4%; industrial cigarettes).20 These data corroborate other reports in the literature and were expected, since 85-90% of the population in Santa Catarina State are Caucasians (light-skinned), besides the fact that smoking increases the risk of this tumor 25-fold.20 Another important finding was that 43.4% of the individuals had a positive family history of skin cancer, since the risk of genetically transmitted predisposition is 50% per gestation, independently of gender, as previously demonstrated.21
Exposure to natural or artificial UV radiation is the risk factor most closely related to the development of SCC, so solar exposure should be avoided between 10:00 AM and 4:00 PM, when UV rays are the strongest (although many individuals that work during this period are unable to avoid it). In our sample, 82.6% of the patients reported solar exposure during this six-hour period, which can explain the tumor’s predominance on surfaces unprotected from sunlight (78.3%), such as the head, neck, and backs of the hands, corroborating data from the literature.22
Therefore, chemical and physical protection from sunlight play a crucial role in the prevention of this cancer. Sunscreen protects the skin by absorption or reflection of the UVA and UVB rays, but the difficulty in its use and constant reapplication are factors that decrease its acceptance. The most widely available sunscreen products on the market have to be reapplied every two hours.23 Only 26 (56.5%) of the participants in this study had ever used sunscreen, which may be due to the high cost of the product and the educational issue.23 Physical protective methods such as hats, long clothing, and/or dark glasses were used by 71.7% of the participants.
Non-melanoma skin tumors are treated as chronic conditions without significant morbidity, but the sequelae from the disease and/or treatment can jeopardize the individual’s psychosocial interaction, negatively influencing OoL.6,24 There are generic questionnaires (SF-36 and WHOQoL) and specific dermatological questionnaires (DLQI and SCI-Skin Cancer Index), which use QoL scores and associated factors, but thus far there is no gold standard in-strument.12,25 The DLQI, used in this study, readily assesses chronic conditions and is validated in the Portuguese language, although it does not capture the patient’s concern with recurrence or emergence of new lesions. The mean score in our sample was 4.02, higher than in other studies, such as Blackford (DLQI: 0.5) and Rhee (DLQI: 1.8), but these authors also included patients with premalignant lesions and BCC along with SCC. 6,26,27
When we categorized the DLQI scores, we found that 23.9% of the tumors had a moderate to severe impact on the individuals’ quality of life, while Steinbauer et al. reported 31%.28 In Nunes et al., who assessed only BCC, the proportion was 10.3%, possibly because this tumor is less agressive.29 We also observed that treatment of tumor (33%) and changes in activities of daily living (30) caused by the skin tumor had a negative influence on QoL. Steinbauer28 and Blackford26 found impairment in terms of symptoms and feelings, leisure-time activities, and activities of daily living.
The literature shows that skin tumors with ulceration, bleeding, signs of growth, or diameter greater than 2cm negatively affect DLQI scores. 30 According to Mallon et al., women with lesions on the face and that undergo disfiguring treatment run greater risk of psychosocial dysfunction. Meanwhile, Shah & Coates applied the DLQI and the Hospital Anxiety and Depression Scale (HADS) and found that patients with ulcerated lesions scored worse on quality of life.31–34 Therefore, the tumor’s appearance and visibility can affect the patient’s wellbeing, but use of sunscreen can have a positive influence.22,35 We did not find any unique variable associated with altered quality of life.
Cancers located on visible areas, especially the face, do not show a significant improvement in QoL after treatment, except for tumors of the lip, which may be related to the functional aesthetic aspect.35 In the assessment of 183 patients with facial lesions (before and following treatment for four months), the DLQI and SCI showed that factors associated with better post-treatment QoL were female gender, age < 50 years, primary lesions, and being employed.35 Importantly, preoccupations with facial scars and aesthetics are increasingly common in contemporary society.
Chen et al.36, assessed patients in the pre and post-operative periods using Skindex-16 and found that individuals with tumors <1cm and in non-photoexposed areas presented better QoL before treatment. One study that included non-melanoma skin tumors found that low income also predicted significant improvement in QoL after treatment, while another study using a generic scale (SF-36) found a minimal impact in patients with initial diagnosis of non-melanoma skin cancer.35 It is possible that generic questionnaires are unable to assess the real influence of skin diseases on QoL.
There is no evidence to date that the tumor’s subtype or demographic characteristics independently predict post-operative QoL, which is not true in the pre-operative assessment. When we used DLQI prior to surgical resection and identified patients with moderate to severe impact on QoL, they were all males, had facial lesions, and were in their fifties (Graph 2). This corroborates the discussion above and findings from the literature in various studies that used this same questionnaire.
There is no gold standard for assessing QoL in dermatological patients, but the DLQI is a good instrument for assessing quality of life in individuals with skin cancer, although it was not created specifically for this purpose.37 There are other limitations, for example that the sample did not include immunosuppressed patients and/or those with relapsed lesions, besides the cross-sectional design. A longitudinal design and pre- and pos-operative follow-up could establish a relationship between the variables at these different time points, but this was not the purpose of the study.
ConclusionIn this sample of patients with clinical and histopathological diagnosis of SCC, we showed a predominance of elderly males with low schooling and low socioeconomic status, working in outdoor activities, with Fitzpatrick phototype II, and with tumors located on the head and neck. One-fourth of the patients presented a moderate to severe negative effect on quality of life prior to the surgical procedure, in addition to a negative influence from the disease on daily activities (33% of cases), treatment effects (30%), and symptoms and feelings (29%).